Accurate medical billing invoice verification requires essential documents such as the patient's insurance information, itemized medical bills, and detailed treatment records. Healthcare providers must also include authorization forms, payment receipts, and any correspondence related to the billing process. Ensuring these documents are complete and accurate streamlines claims processing and reduces the risk of denial or delays.
What Documents are Needed for Medical Billing Invoice Verification?
| Number | Name | Description |
|---|---|---|
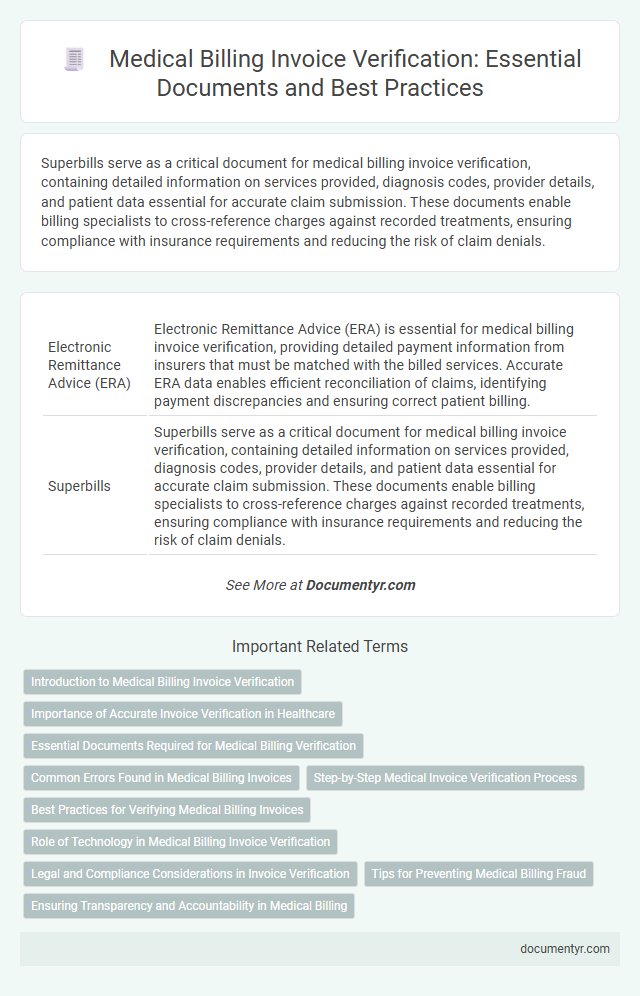
| 1 | Electronic Remittance Advice (ERA) | Electronic Remittance Advice (ERA) is essential for medical billing invoice verification, providing detailed payment information from insurers that must be matched with the billed services. Accurate ERA data enables efficient reconciliation of claims, identifying payment discrepancies and ensuring correct patient billing. |
| 2 | Superbills | Superbills serve as a critical document for medical billing invoice verification, containing detailed information on services provided, diagnosis codes, provider details, and patient data essential for accurate claim submission. These documents enable billing specialists to cross-reference charges against recorded treatments, ensuring compliance with insurance requirements and reducing the risk of claim denials. |
| 3 | Patient Encounter Forms | Patient encounter forms are essential documents for medical billing invoice verification, as they detail the services provided during a patient visit, including diagnoses, procedures, and provider signatures. Accurate patient encounter forms ensure compliance with insurance requirements and facilitate the validation of billed amounts against documented medical services. |
| 4 | Advanced Beneficiary Notice (ABN) | The Advanced Beneficiary Notice (ABN) is a critical document required for medical billing invoice verification, ensuring patients acknowledge potential non-coverage of specific services by Medicare. This form must be accurately completed and signed before billing to prevent claim denials and facilitate transparency in patient financial responsibility. |
| 5 | Prior Authorization Documentation | Prior authorization documentation is essential for medical billing invoice verification as it confirms insurer approval for specific procedures or treatments, preventing claim denials. This documentation typically includes the prior authorization number, approval dates, patient details, and the scope of approved services, ensuring accurate verification and timely reimbursement. |
| 6 | Explanation of Benefits (EOB) | The Explanation of Benefits (EOB) is essential for medical billing invoice verification as it details the services covered, payment amounts, and patient responsibility, ensuring accuracy and transparency. This document helps verify claims against billed charges, preventing errors and facilitating insurance reimbursement. |
| 7 | ICD-10 CM Coding Sheets | Accurate medical billing invoice verification requires ICD-10 CM coding sheets to precisely classify diagnoses and procedures, ensuring compliance with healthcare regulations and facilitating insurance claim approvals. These coding sheets link clinical information with billing data, reducing errors and expediting reimbursement processes. |
| 8 | Charge Master Files | Charge Master Files are essential documents for medical billing invoice verification, containing comprehensive lists of billable services, procedures, and associated costs used to ensure accurate charge capture. These files facilitate validation by cross-referencing billed items with standardized pricing and coding information, reducing errors and discrepancies in the invoice audit process. |
| 9 | Denial Management Logs | Denial management logs are essential documents needed for medical billing invoice verification as they track claim rejections and provide detailed reasons for denials, enabling accurate resubmission and resolution. These logs help identify billing errors, insurance issues, and patient eligibility problems critical for efficient invoice reconciliation and revenue recovery. |
| 10 | Telehealth Consent Forms | Telehealth consent forms are essential documents required for medical billing invoice verification to confirm patient authorization for remote healthcare services. These forms ensure compliance with insurance policies and verify that telehealth services rendered are properly documented for reimbursement. |
Introduction to Medical Billing Invoice Verification
Medical billing invoice verification ensures accuracy and compliance in healthcare payments. It involves reviewing documentation to confirm billing details align with medical services provided.
- Patient Information - Includes identification, insurance details, and contact information to confirm the recipient of services.
- Medical Records - Contains physician notes, treatment descriptions, and diagnosis codes to validate billed procedures.
- Billing Statements - Lists charges, codes, and payment requests required to cross-check financial accuracy.
Your careful submission of these documents helps streamline the verification process and reduces billing errors.
Importance of Accurate Invoice Verification in Healthcare
Accurate invoice verification is critical in healthcare to ensure proper billing and avoid costly errors. The process requires detailed documentation to confirm the validity of medical services billed.
Essential documents for medical billing invoice verification include the patient's medical records, treatment reports, and physician's notes. Insurance authorization forms and payment receipts also play a key role in confirming the accuracy of charges.
Essential Documents Required for Medical Billing Verification
Medical billing invoice verification requires specific documentation to ensure accuracy and compliance. Essential documents help validate services rendered and facilitate smooth reimbursement processes.
- Patient Information - Includes the patient's full name, date of birth, and insurance details to correctly identify the individual.
- Provider Details - Contains the healthcare provider's name, address, and National Provider Identifier (NPI) for proper billing attribution.
- Detailed Service Description - Lists all procedures performed with corresponding CPT or HCPCS codes and dates of service for precise invoicing.
Common Errors Found in Medical Billing Invoices
Accurate document submission is crucial for medical billing invoice verification. Common errors often delay processing and reimbursement.
- Missing Patient Information - Incomplete or incorrect patient details can lead to claim denials.
- Incorrect CPT or ICD Codes - Using outdated or wrong procedure and diagnosis codes causes billing inaccuracies.
- Improper Documentation of Services - Lack of detailed service descriptions may result in rejected or adjusted invoices.
Step-by-Step Medical Invoice Verification Process
Medical billing invoice verification requires specific documents to ensure accurate processing. Key documents include the patient's medical records, billing statements, and insurance details.
Begin the verification process by cross-checking the invoice against the patient's medical records. This step confirms that the services billed match the treatments provided.
Next, verify insurance information to validate coverage and payment terms. Accurate insurance details help prevent claim denials and payment delays.
Finally, review the billing codes and charges on the invoice for accuracy and compliance. Ensuring correct coding reduces errors and streamlines reimbursement.
Best Practices for Verifying Medical Billing Invoices
Medical billing invoice verification requires essential documents such as patient medical records, insurance claim forms, and detailed billing statements. Verifying codes like CPT, ICD-10, and modifiers ensures accuracy in medical billing invoices. Maintaining organized documentation and cross-referencing charges optimizes the verification process and prevents claim denials.
Role of Technology in Medical Billing Invoice Verification
| Document Type | Description | Role of Technology |
|---|---|---|
| Patient Information Form | Contains personal details and insurance information essential for billing. | Electronic Health Records (EHR) systems automate data capture, reducing errors and enhancing accuracy. |
| Medical Service Documentation | Includes physician notes, treatment records, and diagnostic reports that justify the billed services. | Digital imaging and secure cloud storage facilitate easy access and verification of service details by billing software. |
| Insurance Claim Forms | Submitted to insurers to request payment based on the provided medical services. | Automated claim management tools validate information against insurance policies, speeding up the verification process. |
| Payment Receipts and Remittance Advice | Proof of payments received and explanations for any denials or adjustments. | Integrated billing platforms provide real-time updates and reconciliation, ensuring accurate tracking of payments. |
| Authorization and Referral Letters | Documents confirming prior approvals or referrals required for specific treatments. | Electronic authorization systems streamline approval workflows, reducing delays during invoice verification. |
| Technology enhances accuracy and efficiency in medical billing invoice verification by automating data integration, reducing manual errors, and providing secure access to essential documents. Leveraging these digital tools ensures your medical billing process is transparent and compliant. | ||
Legal and Compliance Considerations in Invoice Verification
Medical billing invoice verification requires specific documents to ensure accuracy and compliance with legal standards. Key documents include the patient's insurance information, detailed service records, and authorization forms.
Legal and compliance considerations emphasize the importance of maintaining patient confidentiality through HIPAA regulations and adhering to accurate coding standards such as ICD-10 and CPT. Verification processes must confirm that all services billed are documented and medically necessary. Proper documentation helps prevent fraud, reduces claim denials, and supports audit readiness.
Tips for Preventing Medical Billing Fraud
For medical billing invoice verification, essential documents include the patient's medical records, itemized billing statements, and insurance claim forms. Accurate cross-checking of these documents helps detect discrepancies and prevent fraudulent claims. You should regularly verify provider credentials and service details to ensure all charges are legitimate and authorized.
What Documents are Needed for Medical Billing Invoice Verification? Infographic