Healthcare claims invoice approval requires essential documents including the detailed medical invoice, patient identification, and proof of service such as treatment records or physician notes. Insurance policy information and authorization forms must be included to verify coverage eligibility. Accurate documentation ensures compliance with regulatory standards and facilitates timely processing of healthcare payments.
What Documents Are Necessary for Invoice Approval in Healthcare Claims?
| Number | Name | Description |
|---|---|---|
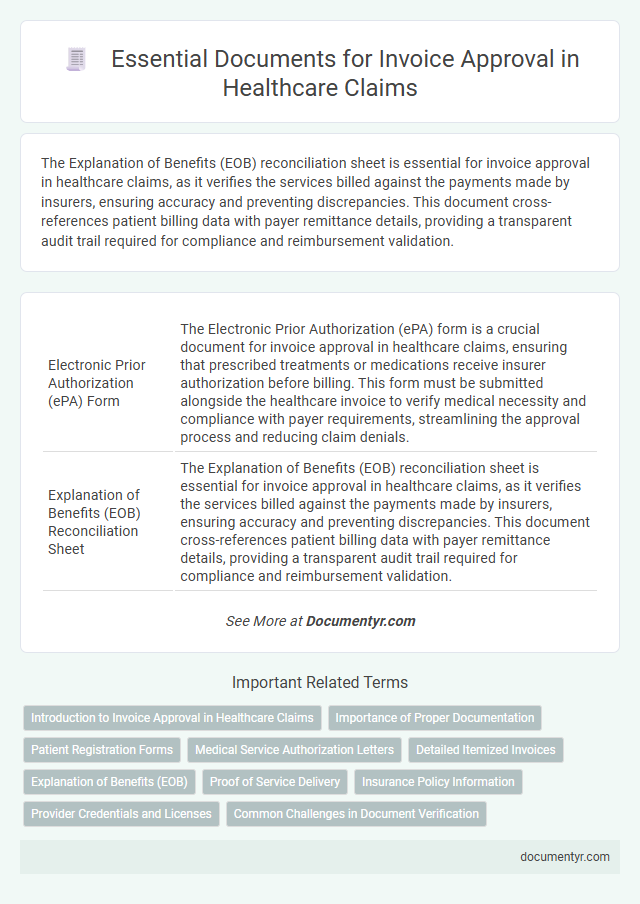
| 1 | Electronic Prior Authorization (ePA) Form | The Electronic Prior Authorization (ePA) form is a crucial document for invoice approval in healthcare claims, ensuring that prescribed treatments or medications receive insurer authorization before billing. This form must be submitted alongside the healthcare invoice to verify medical necessity and compliance with payer requirements, streamlining the approval process and reducing claim denials. |
| 2 | Explanation of Benefits (EOB) Reconciliation Sheet | The Explanation of Benefits (EOB) reconciliation sheet is essential for invoice approval in healthcare claims, as it verifies the services billed against the payments made by insurers, ensuring accuracy and preventing discrepancies. This document cross-references patient billing data with payer remittance details, providing a transparent audit trail required for compliance and reimbursement validation. |
| 3 | Charge Master Validation Report | Charge Master Validation Report is essential for invoice approval in healthcare claims as it verifies the accuracy of billed services and ensures compliance with the facility's billing guidelines. This report cross-checks submitted charges against the approved charge master database, minimizing errors and reducing claim denials. |
| 4 | Itemized UB-04 or CMS-1500 Attachment | Itemized UB-04 or CMS-1500 attachments are essential for invoice approval in healthcare claims as they provide detailed service descriptions, billing codes, and charge breakdowns required for accurate claim processing. These documents ensure compliance with payer requirements by verifying the legitimacy and completeness of the healthcare services billed. |
| 5 | Medical Necessity Certification Letter | Medical Necessity Certification Letter is a crucial document for invoice approval in healthcare claims, confirming that the treatment or service provided meets clinical guidelines and justifies the expense. Insurers require this letter to validate the necessity of medical procedures before processing payments. |
| 6 | HIPAA-Compliant Patient Consent Form | A HIPAA-compliant patient consent form is essential for invoice approval in healthcare claims as it ensures patient authorization for the release and sharing of protected health information (PHI) during the billing process. This document verifies compliance with privacy regulations, reducing the risk of claim denials due to unauthorized use of patient data. |
| 7 | Provider Credentialing Verification | Provider credentialing verification requires submission of valid medical licenses, board certifications, and proof of malpractice insurance alongside the healthcare claim invoice for approval. Accurate documentation of provider credentials ensures compliance with payer policies and prevents delays in invoice processing. |
| 8 | Automated Claim Adjudication Log | The Automated Claim Adjudication Log in healthcare claims requires essential documents such as patient information, treatment codes, provider credentials, and prior authorization details for invoice approval. Accurate and complete submission of these documents ensures efficient validation and reduces claim processing time. |
| 9 | Denial Management Dispute Packet | Essential documents for invoice approval in healthcare claims include the original claim form, detailed medical records, and the Explanation of Benefits (EOB). The Denial Management Dispute Packet must contain a completed appeal letter, supporting clinical documentation, and any prior authorization or referral information to effectively contest claim denials. |
| 10 | Value-Based Care Adjustment Documentation | Healthcare claims invoice approval requires detailed Value-Based Care Adjustment Documentation, including patient eligibility records, clinical outcomes data, and performance metrics aligned with quality benchmarks. Essential documents also encompass signed provider agreements, cost reconciliation reports, and evidence of compliance with established care pathways to validate adjustment accuracy. |
Introduction to Invoice Approval in Healthcare Claims
Invoice approval in healthcare claims is a critical process that ensures accurate reimbursement for medical services provided. It involves verifying that all submitted charges align with the patient's treatment and insurance policy guidelines.
Essential documents for invoice approval include the patient's medical records, itemized billing statements, and insurance claim forms. These documents provide detailed information on the services rendered, dates of service, and applicable codes such as CPT and ICD-10. Proper documentation helps prevent fraud, reduces processing delays, and supports compliance with healthcare regulations like HIPAA.
Importance of Proper Documentation
| Document Type | Description | Importance for Invoice Approval |
|---|---|---|
| Medical Records | Detailed patient history and treatment reports | Verifies the medical necessity of services billed |
| Physician's Orders | Doctor's prescribed tests, procedures, and medications | Confirms that services correspond to approved treatments |
| Claim Form (CMS-1500 or UB-04) | Standardized forms for submitting healthcare claims | Ensures accurate and uniform billing information |
| Proof of Service Delivery | Time-stamped logs, appointment confirmations, or signatures | Validates that billed services were actually provided |
| Insurance Authorization | Pre-approval documents from the payer | Confirms payer consent for coverage of services rendered |
| Itemized Invoice | Breakdown of each service and charge | Facilitates review and auditing of billed amounts |
| Billing Provider's Credentials | Licenses and certifications of healthcare providers | Validates eligibility to bill for healthcare services |
The importance of proper documentation cannot be overstated for invoice approval in healthcare claims. Accurate and comprehensive records support the legitimacy of claims, reduce delays, and minimize the risk of denials. You must ensure all necessary documents are organized and submitted promptly to achieve smooth processing and timely reimbursement.
Patient Registration Forms
```htmlWhat documents are necessary for invoice approval in healthcare claims? Patient registration forms are essential as they verify the patient's identity and insurance details. These forms ensure accurate billing and smooth processing of your healthcare invoices.
```Medical Service Authorization Letters
Medical Service Authorization Letters are crucial documents required for invoice approval in healthcare claims. These letters confirm pre-approval for specific medical services, ensuring compliance and payment authorization.
- Authorization Verification - Confirms that the requested medical service has been pre-approved by the insurer or relevant authority.
- Service Details - Specifies the type of medical service, duration, and any conditions tied to the authorization.
- Patient Identification - Links the authorization letter to the specific patient and treatment plan to prevent billing errors.
Your invoice processing depends on submitting accurate Medical Service Authorization Letters to validate your healthcare claim.
Detailed Itemized Invoices
Detailed itemized invoices are essential documents for invoice approval in healthcare claims. These invoices must include comprehensive descriptions of services rendered, individual costs, and corresponding dates of service. Ensuring your invoice contains this level of detail facilitates accurate claim processing and timely reimbursement.
Explanation of Benefits (EOB)
Invoice approval in healthcare claims requires several essential documents to ensure accurate payment. One of the most critical documents is the Explanation of Benefits (EOB), which details the insurer's payment decisions regarding your claims.
The EOB provides a breakdown of services covered, amounts paid, and any patient responsibility. This document serves as a key reference for verifying charges and resolving discrepancies during the invoice approval process.
Proof of Service Delivery
Proof of service delivery is essential for invoice approval in healthcare claims, verifying that the provided medical services were actually rendered. Accurate documentation ensures timely reimbursement and compliance with regulatory requirements.
- Patient Encounter Records - Detailed notes and signatures from healthcare providers confirming the date, time, and nature of services delivered.
- Service Delivery Receipts - Official receipts or acknowledgments signed by the patient or authorized representative as evidence of service completion.
- Electronic Health Records (EHR) - Digital documentation detailing clinical interventions and treatment outcomes that support the invoice claim.
Insurance Policy Information
Insurance policy information is a critical document necessary for invoice approval in healthcare claims. It verifies coverage details and ensures the services billed align with the insured benefits.
You must provide accurate policy numbers, patient information, and coverage dates to avoid delays in claim processing. This data helps insurers validate eligibility and payment responsibilities effectively.
Provider Credentials and Licenses
Invoice approval in healthcare claims requires thorough verification of provider credentials and licenses to ensure compliance and accuracy. Proper documentation supports legitimacy and facilitates timely payment processing.
- Valid Medical License - Confirms the healthcare provider is legally authorized to deliver medical services within their jurisdiction.
- Board Certification Records - Demonstrate the provider's specialized qualifications and adherence to professional standards.
- National Provider Identifier (NPI) - A unique identification number essential for billing and validating provider identity in healthcare transactions.
What Documents Are Necessary for Invoice Approval in Healthcare Claims? Infographic