To process medical invoice claims for pet care, essential documents include the original invoice detailing the treatments and services provided, a valid prescription or referral from a licensed veterinarian, and proof of payment such as a receipt or bank statement. Accurate pet identification documents like registration or microchip information may also be necessary to verify eligibility. Ensuring all paperwork is complete and matches insurance policy requirements helps expedite claim approval.
What Documents Are Required for Medical Invoice Claims?
| Number | Name | Description |
|---|---|---|
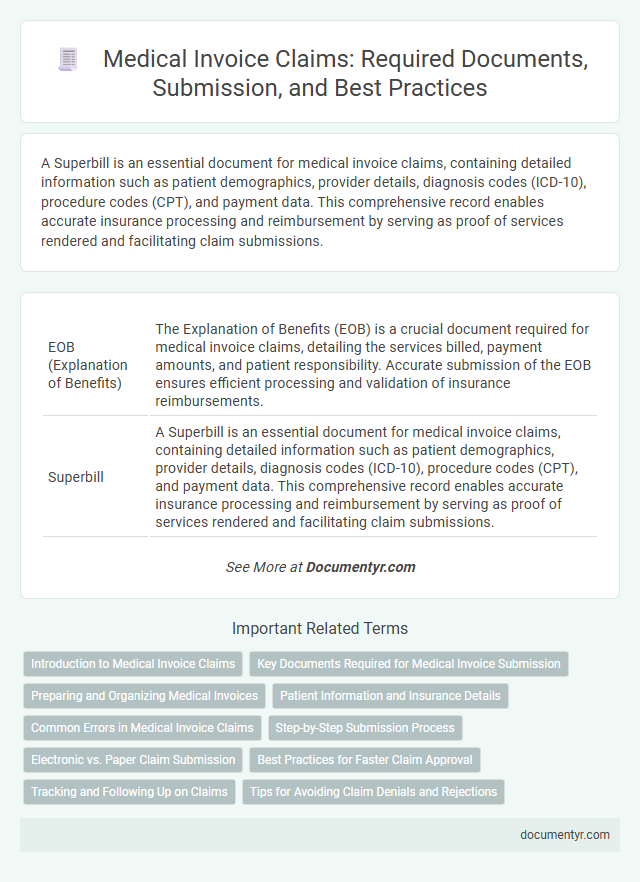
| 1 | EOB (Explanation of Benefits) | The Explanation of Benefits (EOB) is a crucial document required for medical invoice claims, detailing the services billed, payment amounts, and patient responsibility. Accurate submission of the EOB ensures efficient processing and validation of insurance reimbursements. |
| 2 | Superbill | A Superbill is an essential document for medical invoice claims, containing detailed information such as patient demographics, provider details, diagnosis codes (ICD-10), procedure codes (CPT), and payment data. This comprehensive record enables accurate insurance processing and reimbursement by serving as proof of services rendered and facilitating claim submissions. |
| 3 | Pre-authorization Letter | A Pre-authorization Letter is a critical document required for medical invoice claims, as it confirms prior approval from the insurance provider for specific treatments or procedures. This letter ensures that the medical services rendered are eligible for reimbursement and helps prevent claim denials during the payment process. |
| 4 | ICD-10 Code Sheet | Medical invoice claims require an ICD-10 code sheet to accurately document diagnoses and procedures, ensuring proper billing and reimbursement. This standardized coding sheet facilitates precise health condition identification and complies with insurance providers' submission guidelines. |
| 5 | Itemized Bill Summary | An itemized bill summary is essential for medical invoice claims as it details each service, procedure, medication, and supply with corresponding costs, dates, and provider information. This document ensures transparency and accuracy, facilitating verification by insurance companies and expediting reimbursement processes. |
| 6 | Prior Consent Form | The prior consent form is a crucial document required for medical invoice claims, as it verifies the patient's authorization for specific medical procedures and treatments. This form ensures compliance with insurance policies and facilitates the smooth processing and approval of claims. |
| 7 | CPT Coding Report | Accurate CPT coding reports are essential for medical invoice claims, as they provide standardized procedure codes that ensure correct billing and reimbursement. These reports must be submitted alongside itemized bills and physician notes to verify the medical services rendered. |
| 8 | Digital Health Record Extract | Medical invoice claims require the Digital Health Record Extract to provide accurate patient history, treatment details, and service dates. This extract ensures seamless verification and reduces processing time by digitally validating healthcare services rendered. |
| 9 | Telemedicine Session Proof | Telemedicine medical invoice claims require proof of the session, such as an appointment confirmation, session recording, or a detailed consultation summary signed by the healthcare provider. Supporting documents must also include patient identification and the healthcare provider's license to validate the telemedicine service for insurance reimbursement. |
| 10 | Blockchain Timestamp Certificate | For medical invoice claims, a Blockchain Timestamp Certificate offers an immutable and verifiable record of the invoice's creation date, enhancing the authenticity of submitted documents. This certificate supports claims by securely validating the time-sensitive nature of medical services and billing information, reducing disputes and fraud. |
Introduction to Medical Invoice Claims
| Topic | Details |
|---|---|
| Introduction to Medical Invoice Claims | Medical invoice claims involve submitting detailed billing documents to insurance companies or healthcare payers to receive reimbursement for medical services. These claims must include accurate and complete information to ensure a smooth processing and approval. |
| Key Documents Required |
|
| Importance of Accurate Documentation | Providing complete and precise documentation minimizes claim rejections and delays. Clear medical invoices combined with supporting documents improve chances for timely compensation from insurers. |
Key Documents Required for Medical Invoice Submission
Key documents required for medical invoice submission include the original medical invoice, detailed treatment records, and a valid doctor's prescription. These documents verify the authenticity of the medical services provided and the accuracy of the billed amount. Ensuring all necessary paperwork is accurately submitted speeds up the claims processing and approval.
Preparing and Organizing Medical Invoices
Preparing and organizing medical invoices requires collecting essential documents such as the original medical bills, detailed treatment reports, and payment receipts. Accurate patient information and insurance policy details must be included to ensure smooth claim processing. Properly categorized and complete documentation helps avoid delays and facilitates faster reimbursement from insurance providers.
Patient Information and Insurance Details
Accurate patient information is essential for processing medical invoice claims, including the full name, date of birth, and contact details. This data ensures the correct identification of the claimant and prevents delays in reimbursement.
Insurance details such as policy number, insurer's name, and coverage specifics must be clearly documented. These details verify eligibility and determine the extent of claim approval under the patient's insurance plan.
Common Errors in Medical Invoice Claims
Medical invoice claims require precise documentation to ensure smooth processing and avoid delays. Understanding common errors helps you submit accurate claims and receive timely reimbursements.
- Incomplete documentation - Missing medical records or signatures can cause claim denials or delays.
- Incorrect patient information - Errors in patient details such as name, date of birth, or insurance ID result in rejected claims.
- Unclear billing codes - Using wrong or outdated CPT and ICD codes leads to payment disputes and processing issues.
Step-by-Step Submission Process
What documents are required for medical invoice claims? Medical invoice claims typically require a detailed invoice from the healthcare provider, including patient information, dates of service, and itemized charges. Supporting documents such as prescriptions, diagnostic reports, and proof of payment may also be necessary.
How do you begin the submission process for medical invoice claims? Start by gathering all relevant medical documents and invoices related to the treatment or service received. Ensure that each document is accurate and clearly legible to avoid delays in claim processing.
What is the next step after collecting the necessary documents? Fill out the claim form provided by your insurance company or relevant health authority. Include detailed information that matches the invoices and medical records to ensure consistency and accuracy.
Where should the completed medical invoice claim be submitted? Submit all documents and the completed claim form through the insurance provider's designated channels, such as their online portal, email, or physical mailing address. Verify submission guidelines to comply with deadlines and format requirements.
How is the claim status tracked after submission? Use the claim reference number or tracking system provided by the insurance company to monitor the status of your medical invoice claim. Promptly respond to any requests for additional information to facilitate faster processing.
Electronic vs. Paper Claim Submission
Medical invoice claims require specific documentation to ensure accurate processing and reimbursement. Understanding the differences between electronic and paper claim submissions is essential for healthcare providers and patients.
- Electronic Claims Submission - Requires digital forms like the CMS-1500 or UB-04 transmitted via secure electronic data interchange (EDI) systems.
- Paper Claims Submission - Involves physical copies of completed claim forms, which must be mailed or faxed to the insurance payer.
- Supporting Documentation - Both methods require attached medical records, itemized bills, and proof of patient eligibility for claim validation.
Timely and accurate documentation tailored to the chosen submission method helps avoid claim denials and accelerates reimbursement.
Best Practices for Faster Claim Approval
Submitting medical invoice claims requires accurate and complete documentation to ensure timely processing. Essential documents include the original medical invoice, detailed treatment records, and proof of payment.
Best practices for faster claim approval involve double-checking all submitted documents for accuracy and completeness before submission. Including itemized bills and physician's prescriptions can reduce delays caused by verification. Maintaining organized records allows for quick retrieval in case additional information is requested by the insurance provider.
Tracking and Following Up on Claims
Accurate documentation is essential for medical invoice claims to ensure proper tracking and timely processing. Required documents typically include the original invoice, medical reports, and proof of payment.
Keeping copies of all submissions helps you monitor the status of your claim effectively. Regular follow-ups with the insurance provider can prevent delays and resolve discrepancies quickly.
What Documents Are Required for Medical Invoice Claims? Infographic