Medical billing invoice submission requires key documents such as the itemized invoice detailing services provided, patient identification information, and the healthcare provider's credentials. Insurance claim forms, proof of service delivery, and authorization letters or referrals must also be included to ensure accurate processing. Maintaining thorough medical records and billing codes further supports timely reimbursement and compliance with regulations.
What Documents are Necessary for Medical Billing Invoice Submission?
| Number | Name | Description |
|---|---|---|
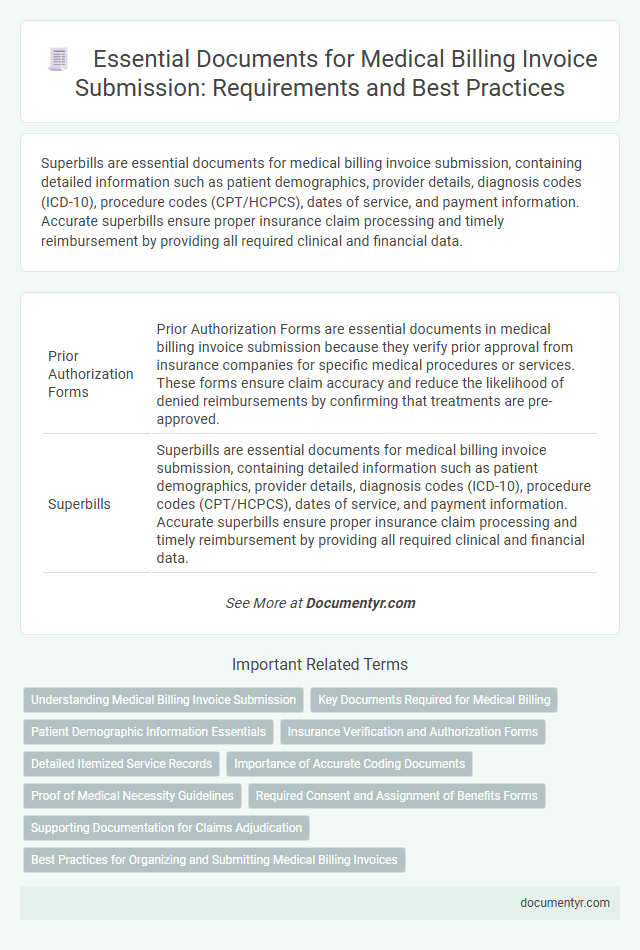
| 1 | Prior Authorization Forms | Prior Authorization Forms are essential documents in medical billing invoice submission because they verify prior approval from insurance companies for specific medical procedures or services. These forms ensure claim accuracy and reduce the likelihood of denied reimbursements by confirming that treatments are pre-approved. |
| 2 | Superbills | Superbills are essential documents for medical billing invoice submission, containing detailed information such as patient demographics, provider details, diagnosis codes (ICD-10), procedure codes (CPT/HCPCS), dates of service, and payment information. Accurate superbills ensure proper insurance claim processing and timely reimbursement by providing all required clinical and financial data. |
| 3 | Explanation of Benefits (EOB) | Explanation of Benefits (EOB) is an essential document for medical billing invoice submission, detailing the insurance provider's payment decisions, patient responsibility, and covered services. This document verifies claim processing accuracy and supports the invoice by itemizing services rendered, payment amounts, denials, and adjustments required for accurate billing reconciliation. |
| 4 | Clearinghouse Rejection Reports | Medical billing invoice submission requires essential documents such as detailed patient information, itemized service records, and the insurance claim form; Clearinghouse rejection reports must be reviewed meticulously to identify errors in coding, patient data, or insurance details. Addressing issues highlighted in these rejection reports ensures accurate resubmission, reduces claim denials, and accelerates reimbursement processes. |
| 5 | Referral Letters | Referral letters are essential documents for medical billing invoice submission as they verify the necessity of specialized services and ensure compliance with insurance requirements. Including accurate referral letters prevents claim denials and accelerates payment processing by providing clear authorization from the referring physician. |
| 6 | Electronic Data Interchange (EDI) Files | Medical billing invoice submission requires Electronic Data Interchange (EDI) files such as the 837 healthcare claim transaction, which contains patient information, diagnosis codes, and billing details. Supporting documents like the 835 remittance advice and prior authorization forms must be accurately linked to ensure compliance and prompt insurance reimbursement. |
| 7 | HIPAA-Compliant Patient Consent Forms | HIPAA-compliant patient consent forms are essential documents for medical billing invoice submission, ensuring that all patient information is authorized for use and disclosure in billing processes. These forms protect patient privacy by explicitly granting permission to share medical and billing details with insurance providers and billing entities. |
| 8 | ICD-10 and CPT Code Validation Sheets | Accurate submission of medical billing invoices requires ICD-10 and CPT code validation sheets to ensure proper diagnosis and procedure coding, directly affecting claim approval and reimbursement rates. These documents verify the alignment of medical services with standardized coding systems, reducing errors and facilitating seamless insurance processing. |
| 9 | Provider NPI Attestation | The Provider NPI Attestation is essential for medical billing invoice submission, confirming the accuracy and legitimacy of the provider's National Provider Identifier. This document ensures compliance with regulatory requirements and facilitates the efficient processing of claims by verifying the provider's credentials. |
| 10 | Payor-Specific Incident-to Documentation | Accurate Payor-Specific Incident-to Documentation requires detailed provider notes, proof of physician supervision, and a valid treatment plan aligned with payer guidelines to ensure claim approval. Submission must include properly coded visit notes, evidence of incident-to eligibility, and any required prior authorizations specific to the insurance provider's policies. |
Understanding Medical Billing Invoice Submission
| Document Type | Description | Importance in Medical Billing Invoice Submission |
|---|---|---|
| Patient Information Form | Includes patient's personal details, insurance information, and consent forms. | Ensures correct patient identification and insurance verification for accurate billing. |
| Medical Records | Detailed notes and documentation of the diagnosis, treatment, and clinical procedures performed. | Supports the medical necessity of the services billed and substantiates claims to insurance providers. |
| Physician's Order or Prescription | Written or electronic orders that authorize specific treatments or diagnostic tests. | Verifies legitimacy of provided services, critical for claim approvals. |
| Itemized Invoice or Billing Statement | A comprehensive list of billed services, including CPT codes, dates of service, and charges. | Facilitates transparent and accurate invoicing, streamlining payment processing. |
| Insurance Claim Form | Standardized form required by insurance companies to process reimbursement claims. | Acts as the primary document for submitting claims and tracking payment status. |
| Authorization or Referral Document | Prior authorization or referral from a primary care provider when required for specific treatments. | Validates approval for covered services, minimizing claim denials. |
| Explanation of Benefits (EOB) | Statement from the insurance company detailing payment decisions and patient responsibility. | Helps reconcile payments with invoices and identifies outstanding balances. |
| Payment Receipts | Proof of payments received from insurance companies or patients. | Ensures accurate financial record-keeping and reduces billing disputes. |
| Compliance and Regulatory Documentation | Includes HIPAA consent forms and other legal paperwork ensuring data privacy and billing compliance. | Protects patient information and adheres to healthcare billing regulations. |
Key Documents Required for Medical Billing
Key documents required for medical billing invoice submission include the patient's medical records, itemized billing statements, and insurance claim forms. These documents ensure accurate verification of services rendered and facilitate timely insurance processing. Proper documentation reduces claim denials and improves reimbursement efficiency in medical billing.
Patient Demographic Information Essentials
Accurate patient demographic information is crucial for medical billing invoice submission to ensure proper identification and insurance processing. This data helps prevent billing errors and facilitates seamless communication between healthcare providers and payers.
- Full Name - The patient's legal name must be recorded to correctly identify the individual on the invoice.
- Date of Birth - Essential for verifying patient identity and eligibility for insurance coverage.
- Contact Information - Includes phone number and address, necessary for communication and claim follow-up.
- Insurance Details - Policy numbers and provider information are required to process claims accurately.
- Patient Identification Number - A unique identifier assigned by the healthcare provider or insurance carrier for billing accuracy.
Insurance Verification and Authorization Forms
Medical billing invoice submission requires precise documentation to ensure accurate processing and payment. Two critical documents are the insurance verification and authorization forms.
Insurance verification confirms the patient's coverage details, including policy status, benefits, and co-pay amounts. Authorization forms are necessary to obtain prior approval from the insurance provider for certain medical procedures or services. Submitting these documents minimizes claim denials and accelerates reimbursement.
Detailed Itemized Service Records
Detailed itemized service records are essential for accurate medical billing invoice submission. These records provide a comprehensive breakdown of each service rendered, including dates, procedures, and corresponding costs. Precise documentation ensures correct reimbursement and reduces claim denials from insurance providers.
Importance of Accurate Coding Documents
What documents are necessary for medical billing invoice submission? Accurate coding documents, including the ICD, CPT, and HCPCS codes, are essential for correct claim processing. These codes ensure precise communication of medical services and procedures, reducing the risk of claim denials.
Proof of Medical Necessity Guidelines
Proper documentation is essential for medical billing invoice submission to ensure compliance with Proof of Medical Necessity guidelines. These documents validate the necessity of medical services rendered and support accurate reimbursement claims.
- Physician's Order - A signed order from the attending physician specifying the medical service required.
- Medical Records - Detailed patient records documenting diagnosis, treatment plans, and clinical findings.
- Supporting Test Results - Laboratory or imaging results that confirm the need for the prescribed medical procedure or service.
Submitting these documents with the medical billing invoice reduces claim denials and speeds up payment processing.
Required Consent and Assignment of Benefits Forms
Required consent and assignment of benefits forms are essential documents for medical billing invoice submission. These forms authorize the healthcare provider to bill your insurance directly and share necessary information for claim processing.
Without properly signed consent and assignment of benefits forms, insurance claims may be delayed or denied. Ensuring these documents are complete and accurate helps streamline reimbursement and supports compliance with billing regulations.
Supporting Documentation for Claims Adjudication
Supporting documentation is essential for accurate medical billing invoice submission and successful claims adjudication. Proper documents verify the services provided and ensure compliance with payer requirements.
- Patient Information - Accurate patient details such as name, date of birth, and insurance ID confirm the identity of the insured individual.
- Medical Records - Detailed clinical notes and treatment documentation validate the necessity and scope of the billed services.
- Physician Orders and Authorizations - Official orders and prior authorizations demonstrate payer approval for specific treatments or procedures.
What Documents are Necessary for Medical Billing Invoice Submission? Infographic