Submitting a health insurance appeal requires essential documents such as the original denial letter, a detailed appeal letter explaining the reason for contesting the decision, and relevant medical records supporting the claim. Include any physician's notes, test results, and treatment plans that justify the necessity of the denied service. Ensuring all paperwork is complete and well-organized improves the chances of a successful appeal.
What Documents Are Needed for Submitting a Health Insurance Appeal?
| Number | Name | Description |
|---|---|---|
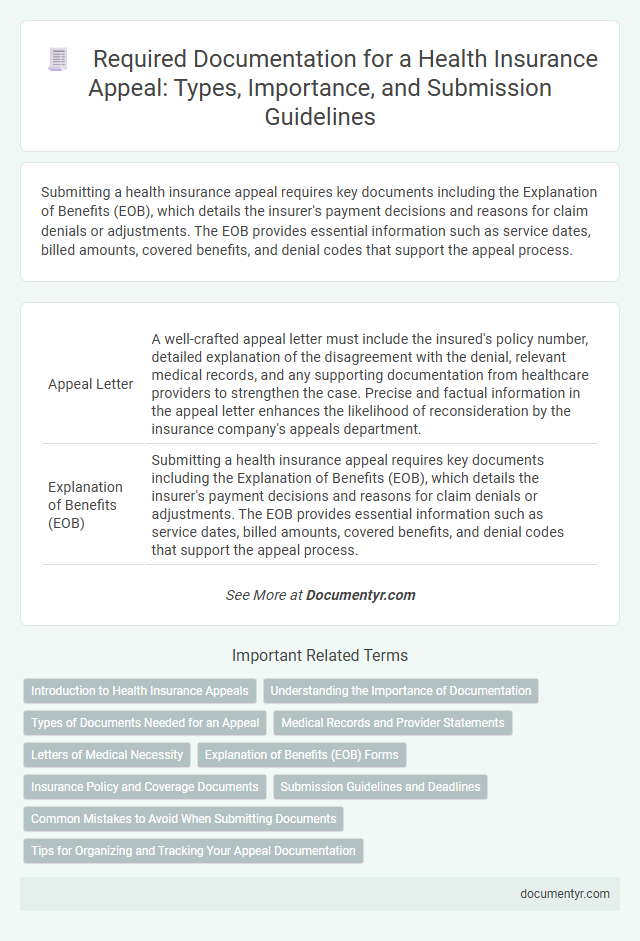
| 1 | Appeal Letter | A well-crafted appeal letter must include the insured's policy number, detailed explanation of the disagreement with the denial, relevant medical records, and any supporting documentation from healthcare providers to strengthen the case. Precise and factual information in the appeal letter enhances the likelihood of reconsideration by the insurance company's appeals department. |
| 2 | Explanation of Benefits (EOB) | Submitting a health insurance appeal requires key documents including the Explanation of Benefits (EOB), which details the insurer's payment decisions and reasons for claim denials or adjustments. The EOB provides essential information such as service dates, billed amounts, covered benefits, and denial codes that support the appeal process. |
| 3 | Denial Letter from Insurer | The denial letter from the insurer is a critical document needed for submitting a health insurance appeal as it outlines the specific reasons for claim denial. Providing this letter helps clarify the insurer's decision and supports the appeal by addressing each cited issue with relevant medical records and expert opinions. |
| 4 | Completed Appeal Form (if applicable) | A completed appeal form is essential for submitting a health insurance appeal as it provides detailed information about the claimant, the disputed claim, and the grounds for contesting the denial. This form ensures that the insurance company can accurately process and evaluate the appeal based on the specific reasons and supporting documentation provided. |
| 5 | Medical Records | Medical records, including detailed physician notes, test results, and hospital discharge summaries, are essential for submitting a health insurance appeal as they provide critical evidence supporting the necessity of the denied treatment. Accurate and complete documentation of diagnoses, treatments, and prescriptions strengthens the appeal by demonstrating compliance with medical guidelines and insurer requirements. |
| 6 | Doctor’s Letter or Medical Necessity Statement | A Doctor's Letter or Medical Necessity Statement is crucial for submitting a health insurance appeal, as it provides detailed clinical reasons justifying the prescribed treatment or service. This document must clearly explain why the treatment is necessary, supported by medical evidence and patient history, to increase the likelihood of overturning a denied claim. |
| 7 | Prescription Records | Prescription records play a crucial role in submitting a health insurance appeal, providing detailed evidence of prescribed medications related to the treatment in question. Including accurate and complete prescription documentation helps demonstrate medical necessity and supports the case for coverage approval. |
| 8 | Itemized Bill from Provider | An itemized bill from the healthcare provider is essential for submitting a health insurance appeal, as it details each service rendered, including dates, descriptions, and costs, allowing insurers to verify the accuracy of claims and charges. This document supports the appeal by clearly identifying discrepancies or errors in billed services that may have led to denial or underpayment. |
| 9 | Referral Letters (if required) | Referral letters are essential documents for submitting a health insurance appeal when the insurer requires proof that a specialist visit or specific treatment was medically necessary and authorized by a primary care physician. These letters must clearly state the medical reason for the referral, the specialist's details, and the authorized approval date to strengthen the appeal's credibility. |
| 10 | Supporting Research or Clinical Guidelines | Submitting a health insurance appeal requires detailed medical records, including clinical notes and test results that align with accepted clinical guidelines such as those from the American Medical Association or National Comprehensive Cancer Network. Supporting research studies, peer-reviewed journal articles, and evidence-based clinical protocols should be included to substantiate the medical necessity and treatment efficacy in the appeal documentation. |
| 11 | Insurance Policy Document | The insurance policy document is essential for submitting a health insurance appeal as it contains the terms, coverage details, and exclusions relevant to the claim dispute. Including this document helps validate the appeal by clearly demonstrating the policyholder's rights and the insurer's obligations under the contract. |
| 12 | Previous Correspondence with Insurer | Including all previous correspondence with the insurer, such as denial letters and communication records, is essential when submitting a health insurance appeal to clearly demonstrate the claim's history and reasons for dispute. Detailed documentation of earlier interactions helps ensure a thorough review and increases the likelihood of a successful appeal resolution. |
| 13 | Authorization Forms | Authorization forms are essential documents required when submitting a health insurance appeal, granting the insurer permission to review medical records and other relevant information. These forms ensure compliance with privacy regulations and expedite the appeal process by allowing access to necessary healthcare data. |
| 14 | Payment Receipts | Payment receipts serve as crucial evidence when submitting a health insurance appeal, clearly documenting premiums paid and transactions related to medical expenses. Including detailed, itemized payment receipts strengthens the appeal by verifying timely payments and supporting claims for denied or delayed reimbursements. |
| 15 | Test Results or Imaging Reports | Test results and imaging reports are crucial documents for submitting a health insurance appeal, as they provide objective medical evidence supporting the necessity of treatment or services. Including detailed lab results, MRI scans, X-rays, and pathology reports increases the likelihood of a successful appeal by clearly demonstrating the medical basis for the claim. |
Introduction to Health Insurance Appeals
Submitting a health insurance appeal requires specific documents to support your case effectively. Understanding the necessary paperwork ensures a smoother and faster review process by the insurance provider.
- Denial Letter - A formal notice from your insurer explaining why your claim was denied.
- Claim Form - The original health insurance claim submitted for coverage or reimbursement.
- Medical Records - Detailed documentation from healthcare providers supporting the medical necessity of the services.
- Physician's Letter - A professional statement from your doctor explaining the treatment and necessity.
- Proof of Payment - Receipts or billing statements confirming payments made towards medical services.
- Insurance Policy - Your health insurance contract outlining coverage terms and conditions.
Understanding the Importance of Documentation
Submitting a health insurance appeal requires specific documentation to support your case effectively. Essential documents include the denial letter from the insurance company, medical records related to the treatment, and a detailed appeal letter explaining the reasons for reconsideration. Proper documentation ensures clarity and strengthens the appeal by providing evidence that justifies coverage or payment adjustments.
Types of Documents Needed for an Appeal
Submitting a health insurance appeal requires specific documents to support your case effectively. Key types of documents include the original denial letter, detailed medical records, and any correspondence with your insurance provider. Collecting these essential papers strengthens the appeal and helps ensure a thorough review process.
Medical Records and Provider Statements
What documents are essential for submitting a health insurance appeal? Medical records provide a detailed account of your diagnosis, treatment, and medical history, which are critical for supporting your appeal. Provider statements offer professional insights and clarifications that can strengthen the case for coverage reconsideration.
Letters of Medical Necessity
When submitting a health insurance appeal, it is crucial to include all relevant documents that support your case. Letters of Medical Necessity are among the most important, as they provide detailed explanations from healthcare providers justifying the need for specific treatments or services.
These letters help the insurance company understand the medical reasons behind the requested care. Ensuring that your appeal contains clear and comprehensive Letters of Medical Necessity increases the likelihood of a successful outcome.
Explanation of Benefits (EOB) Forms
When submitting a health insurance appeal, one of the most important documents is the Explanation of Benefits (EOB) form. This form provides detailed information about the insurance claim, including the services billed, amount covered, and patient responsibility.
The EOB form helps you understand why a claim was denied or partially paid, which is crucial for building a strong appeal. It includes essential details such as claim number, dates of service, and the insurer's reason for denial. Providing a complete and accurate EOB form ensures your appeal is processed efficiently and increases the chances of approval.
Insurance Policy and Coverage Documents
Submitting a health insurance appeal requires specific documents to support your case. Insurance policy and coverage documents are essential to demonstrate the terms and conditions related to your claim.
- Insurance Policy Document - This outlines the coverage details, limits, and exclusions applicable to your health insurance plan.
- Explanation of Benefits (EOB) - Provides a summary of the claim decision, including approved and denied services with reasons.
- Coverage Verification Letter - Confirms the active status and coverage scope of your health insurance during the treatment period.
Including these documents strengthens the validity of your health insurance appeal and aids in a faster review process.
Submission Guidelines and Deadlines
| Document | Description | Submission Guidelines | Deadlines |
|---|---|---|---|
| Appeal Form | Official form provided by the insurance company to initiate the appeal process. | Complete all required fields accurately and submit as instructed by the insurer, either online or by mail. | Typically must be submitted within 60 days from the date of the denial letter. |
| Denial Letter | Formal notification from the insurer explaining the reason for the claim denial. | Include a copy of this letter with your appeal documents to provide context. | Submit alongside the appeal form within the specified appeal period. |
| Medical Records | Relevant health records supporting the necessity of the denied treatment or service. | Ensure records are up-to-date and clearly legible; submit copies, not originals. | Must be included when submitting your appeal to strengthen your case. |
| Physician's Letter | A detailed statement from your healthcare provider justifying the medical necessity of the claimed service. | Obtain a signed letter addressing the denial reasons and attach it to your appeal. | Should accompany the initial appeal submission to avoid delays. |
| Proof of Payment | Receipts or invoices proving that you have paid for the denied service, if applicable. | Submit copies to demonstrate financial responsibility and support your appeal. | Include with appeal documents before the appeal deadline. |
Common Mistakes to Avoid When Submitting Documents
Submitting accurate and complete documents is crucial when filing a health insurance appeal. Common mistakes include missing signatures, incomplete forms, and unclear medical records.
Failing to provide detailed explanations or relevant supporting evidence can lead to delays or denials. Always double-check that all required documents comply with the insurer's guidelines to avoid processing errors.
What Documents Are Needed for Submitting a Health Insurance Appeal? Infographic