Patients must provide identification documents, insurance cards, and detailed medical records, including diagnostic tests and physician notes, for surgery pre-authorization. Authorization forms from the healthcare provider and any referral letters from specialists may also be required. Accurate and complete documentation ensures a smooth approval process and prevents delays in scheduling the surgery.
What Documents Does a Patient Need for Surgery Pre-Authorization?
| Number | Name | Description |
|---|---|---|
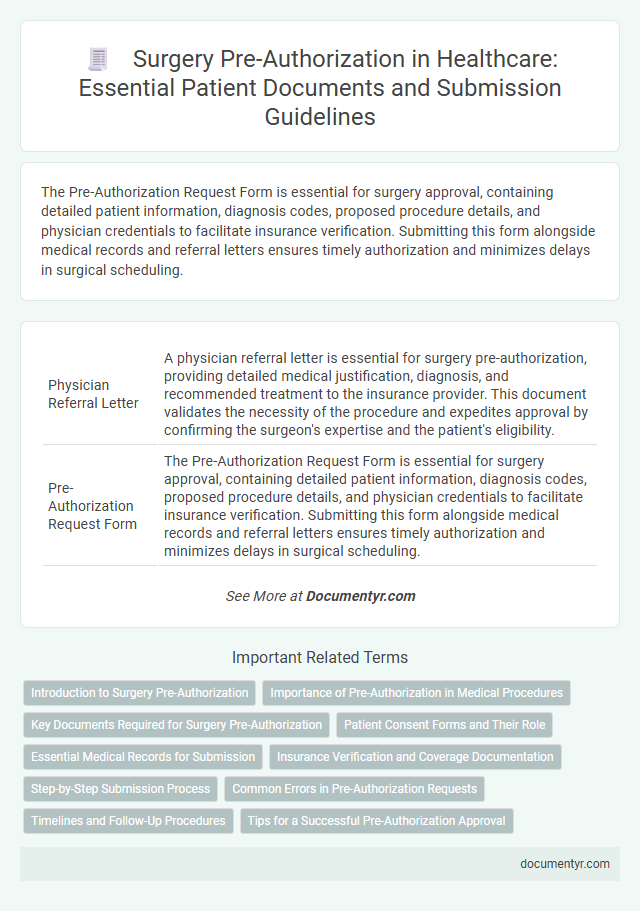
| 1 | Physician Referral Letter | A physician referral letter is essential for surgery pre-authorization, providing detailed medical justification, diagnosis, and recommended treatment to the insurance provider. This document validates the necessity of the procedure and expedites approval by confirming the surgeon's expertise and the patient's eligibility. |
| 2 | Pre-Authorization Request Form | The Pre-Authorization Request Form is essential for surgery approval, containing detailed patient information, diagnosis codes, proposed procedure details, and physician credentials to facilitate insurance verification. Submitting this form alongside medical records and referral letters ensures timely authorization and minimizes delays in surgical scheduling. |
| 3 | Medical History Report | A comprehensive Medical History Report is essential for surgery pre-authorization, detailing past illnesses, surgeries, allergies, and current medications to ensure accurate risk assessment and treatment planning. This document helps insurance providers verify the necessity of the procedure and supports clinicians in optimizing patient care. |
| 4 | Recent Consultation Notes | Recent consultation notes are crucial for surgery pre-authorization as they provide updated clinical findings and validate the medical necessity of the procedure. These notes must include detailed assessments, diagnostic results, and physician recommendations to ensure accurate insurance review and approval. |
| 5 | Current Medication List | A current medication list is essential for surgery pre-authorization as it provides healthcare providers with detailed information on all prescribed, over-the-counter, and herbal medications the patient is taking, helping to prevent adverse drug interactions during surgery. Accurate documentation of dosage, frequency, and medication names ensures a safer surgical plan and compliance with insurance requirements. |
| 6 | Diagnostic Test Results (e.g., X-rays, MRI, CT scans, lab reports) | Diagnostic test results such as X-rays, MRI scans, CT scans, and lab reports are critical documents required for surgery pre-authorization to verify the medical necessity and support the surgical plan. These diagnostic records provide detailed evidence enabling insurance providers to assess risk, justify coverage, and approve the proposed procedure efficiently. |
| 7 | Insurance Information Form | The Insurance Information Form is essential for surgery pre-authorization, containing detailed patient insurance policy numbers, provider contact information, and coverage specifics necessary to verify eligibility and benefits. Accurate completion of this form ensures timely approval by the insurance carrier, preventing delays in surgical scheduling and coverage confirmation. |
| 8 | Surgical Procedure Recommendation | A surgical procedure recommendation from a licensed physician outlining the necessity and specifics of the surgery is essential for surgery pre-authorization. This document must include diagnosis details, proposed treatment plans, and expected outcomes to facilitate insurance approval. |
| 9 | Physician’s Clinical Notes | Physician's clinical notes are essential for surgery pre-authorization as they provide detailed documentation of the patient's diagnosis, treatment history, and medical necessity for the procedure. Comprehensive clinical notes ensure accurate assessment by insurance reviewers, facilitating approval and minimizing delays in surgical care. |
| 10 | Relevant Specialist Reports | Relevant specialist reports such as cardiology evaluations, pulmonary function tests, and endocrinology assessments are essential for surgery pre-authorization to provide detailed medical history and current health status. These documents enable insurance providers to verify the necessity and safety of the procedure based on specialist insights. |
| 11 | Treatment Plan Summary | A detailed Treatment Plan Summary is essential for surgery pre-authorization, outlining the diagnosis, proposed procedure, expected outcomes, and duration of recovery. This document ensures insurance providers assess medical necessity and approve coverage based on comprehensive clinical information. |
| 12 | Consent for Release of Information | A Consent for Release of Information document is essential for surgery pre-authorization as it allows healthcare providers to share medical records with insurance companies for verification and approval. This consent ensures compliance with HIPAA regulations and facilitates timely processing of surgical authorization requests. |
| 13 | Insurance Card Copy | A patient must provide a clear copy of their insurance card, displaying both the front and back, to facilitate verification and pre-authorization for surgery. This document is essential for insurance providers to confirm coverage details and process approvals efficiently. |
| 14 | Patient Identification (ID) | Patients must provide valid government-issued identification, such as a driver's license or passport, to verify their identity during surgery pre-authorization. This ensures accurate matching of medical records and insurance information, facilitating a smooth authorization process. |
| 15 | Primary Care Physician Notes | Primary care physician notes play a crucial role in surgery pre-authorization by providing detailed medical history, current health status, and documented necessity for the procedure. Insurance providers rely heavily on these notes to validate the surgery's medical justification and ensure compliance with policy requirements. |
| 16 | Prior Treatment Records | Prior treatment records, including previous MRI scans, lab results, and specialist consultation notes, are essential for surgery pre-authorization to provide a comprehensive medical history. These documents help insurance providers evaluate the necessity and appropriateness of the surgical procedure based on past treatments and outcomes. |
| 17 | Letter of Medical Necessity | A Letter of Medical Necessity is a critical document required for surgery pre-authorization, detailing the specific medical reasons for the procedure and supporting evidence from the healthcare provider. This letter emphasizes the urgency and necessity of the surgery, facilitating insurance approval by clearly outlining the patient's condition and treatment plan. |
| 18 | Hospital Admission Form (if applicable) | Patients must provide a completed hospital admission form, which includes personal identification, insurance details, and the referring physician's information, to facilitate surgery pre-authorization. This document ensures the hospital verifies patient eligibility and coordinates with insurance providers for coverage approval. |
| 19 | Pre-Surgical Clearance (e.g., cardiology, anesthesia) | Patients require pre-surgical clearance documents from specialists such as cardiology and anesthesia to ensure fitness for surgery, including recent ECG reports, echocardiograms, and anesthesia risk assessments. These documents support insurance pre-authorization by validating the necessity and safety of the procedure. |
Introduction to Surgery Pre-Authorization
What documents does a patient need for surgery pre-authorization? Surgery pre-authorization requires specific medical and insurance documents to ensure approval from your healthcare provider and insurance company. Proper documentation streamlines the authorization process and prevents delays in your surgical procedure.
Importance of Pre-Authorization in Medical Procedures
Pre-authorization for surgery is a critical step in ensuring that medical procedures are covered by insurance and proceed without financial complications. Patients must prepare specific documents to facilitate this authorization and avoid delays in treatment.
The importance of pre-authorization lies in verifying medical necessity, confirming insurance coverage, and preventing unexpected out-of-pocket expenses for patients undergoing surgery.
- Insurance Card - Provides proof of insurance and essential information for verifying coverage eligibility.
- Physician's Referral - Confirms the necessity of surgery and supports the pre-authorization request with relevant medical details.
- Medical Records and Test Results - Demonstrates the patient's condition and justifies the need for the surgical procedure.
Key Documents Required for Surgery Pre-Authorization
Securing surgery pre-authorization requires specific key documents that validate the medical necessity and insurance coverage. These documents ensure the patient's procedure is approved by the insurance provider before the surgery date.
The primary document is the physician's detailed surgical recommendation, outlining the medical condition and necessity of the procedure. Insurance cards and patient identification verify coverage eligibility and identity. Additionally, prior medical records and test results related to the condition may be required to support the pre-authorization request.
Patient Consent Forms and Their Role
Patient consent forms are crucial documents required for surgery pre-authorization. These forms confirm that You understand the procedure, its risks, and benefits before the surgery takes place.
Healthcare providers use consent forms to ensure legal and ethical compliance and to protect patient rights. Without properly signed consent forms, insurance companies may deny pre-authorization and delay surgery scheduling.
Essential Medical Records for Submission
Essential medical records are required for surgery pre-authorization to ensure accurate assessment and approval. These documents typically include your detailed medical history and current diagnostic reports.
Provider notes, surgical plans, and lab results are crucial to demonstrate the necessity of the procedure. Insurance companies rely on this comprehensive information to process authorization efficiently.
Insurance Verification and Coverage Documentation
Before surgery, verifying your insurance coverage is essential for pre-authorization. Proper documentation ensures the procedure is approved and covered by your insurer.
- Insurance Card - Provides essential information including policy number and group ID needed for verification.
- Pre-authorization Form - Completed by your healthcare provider to request surgical approval from the insurance company.
- Coverage Statement - Confirms which procedures and services are included under your insurance plan.
Submitting these documents accurately helps avoid delays in your surgical treatment and guarantees insurance compliance.
Step-by-Step Submission Process
To obtain surgery pre-authorization, you need to gather essential documents including your referral from a primary care physician, medical records detailing your condition, and the surgeon's treatment plan. Submit these documents along with your insurance information and any prior authorizations required by your health plan. Following the submission, monitor your insurance provider's communication for approval status or requests for additional information to ensure timely processing.
Common Errors in Pre-Authorization Requests
Patients must provide accurate and complete documentation to ensure successful surgery pre-authorization. Missing or incorrect documents often cause delays or denials in the pre-authorization process.
- Incomplete Medical Records - Submitting partial or outdated medical records can lead to authorization rejection.
- Incorrect Insurance Information - Providing wrong policy numbers or insurance details causes processing errors.
- Lack of Physician's Certification - Absence of the surgeon's detailed procedure justification affects approval chances.
Timelines and Follow-Up Procedures
Patients must submit essential documents such as a valid ID, insurance information, and a physician's referral to initiate surgery pre-authorization. Pre-authorization timelines typically range from 3 to 10 business days, depending on the insurance provider's review process. Follow-up procedures involve confirming approval status via phone or online portal to avoid surgery delays.
What Documents Does a Patient Need for Surgery Pre-Authorization? Infographic