Patients need to provide a signed authorization form specifying the medical records to be transferred and the receiving facility's details. A valid government-issued ID is often required to verify the patient's identity. Insurance information and any previous medical history documents can facilitate a smoother transfer process.
What Documents Does a Patient Need for Medical Record Transfers?
| Number | Name | Description |
|---|---|---|
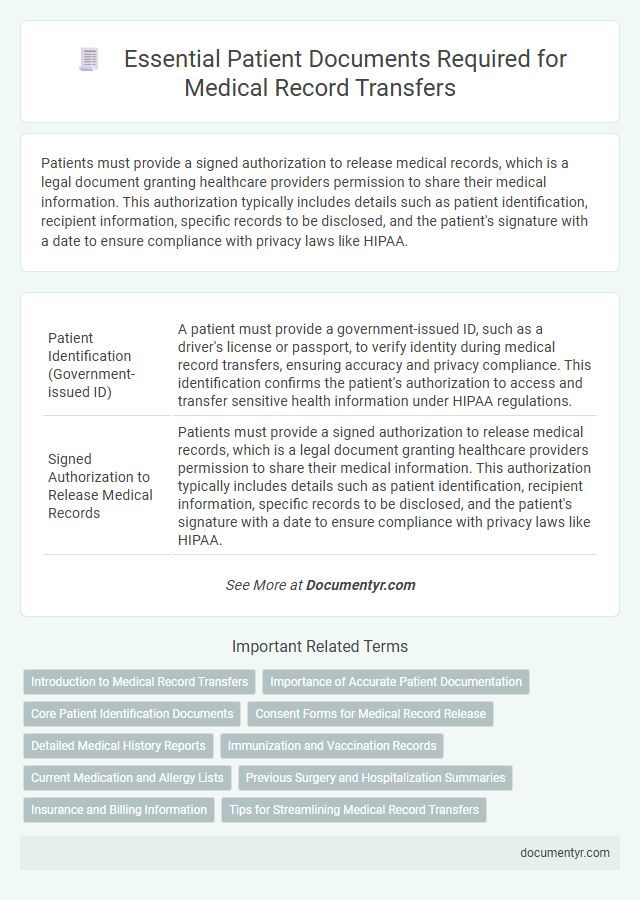
| 1 | Patient Identification (Government-issued ID) | A patient must provide a government-issued ID, such as a driver's license or passport, to verify identity during medical record transfers, ensuring accuracy and privacy compliance. This identification confirms the patient's authorization to access and transfer sensitive health information under HIPAA regulations. |
| 2 | Signed Authorization to Release Medical Records | Patients must provide a signed authorization to release medical records, which is a legal document granting healthcare providers permission to share their medical information. This authorization typically includes details such as patient identification, recipient information, specific records to be disclosed, and the patient's signature with a date to ensure compliance with privacy laws like HIPAA. |
| 3 | Medical Record Transfer Request Form | A Medical Record Transfer Request Form is essential for authorizing the release of a patient's health information to a new healthcare provider, ensuring compliance with HIPAA regulations and protecting patient privacy. This form typically includes patient identification details, previous and receiving provider information, specific records requested, and the patient's signature granting permission for the transfer. |
| 4 | Insurance Information | Patients must provide their current insurance card and policy number to ensure accurate medical record transfers and seamless billing processes. Including detailed insurance provider contact information helps prevent delays in claim submissions and authorizations. |
| 5 | Previous Medical Records Summary | A patient needs to provide a detailed Previous Medical Records Summary, including diagnoses, treatments, medications, and test results, to ensure accurate and comprehensive medical record transfers. This summary allows the receiving healthcare provider to quickly understand the patient's medical history and make informed decisions for ongoing care. |
| 6 | Immunization Records | Patients need to provide official immunization records containing detailed vaccine history, including dates, types, and doses administered, to ensure accurate and complete medical record transfers. These documents are essential for verifying vaccination status and supporting continuity of care across healthcare providers. |
| 7 | Medication List | Patients need to provide an up-to-date medication list including prescription drugs, over-the-counter medications, dosages, and frequency when requesting medical record transfers to ensure accurate continuity of care. A comprehensive medication list helps healthcare providers avoid drug interactions and tailor treatment plans effectively. |
| 8 | Referral Letter (if applicable) | A Referral Letter, if applicable, is a critical document in medical record transfers as it contains detailed information about the patient's diagnosis, treatment history, and reason for referral, ensuring continuity of care. This letter, typically authored by the referring physician, facilitates clear communication between healthcare providers and supports accurate and efficient medical record exchanges. |
| 9 | Advance Directives (if applicable) | Patients must provide copies of advance directives, such as living wills or durable power of attorney for healthcare, to ensure their medical preferences are honored during record transfers. Including these documents in the transfer process guarantees that healthcare providers have access to legally binding instructions related to treatment decisions. |
| 10 | Test Results and Imaging Reports | Patients must provide authorized consent forms along with copies of relevant test results and imaging reports, such as blood tests, X-rays, MRIs, and CT scans, to ensure accurate and complete medical record transfers. These documents allow healthcare providers to review diagnostic information and continue appropriate care without unnecessary repetition of tests. |
| 11 | Surgical Reports (if applicable) | Patients requesting medical record transfers for surgeries must provide detailed surgical reports, which include operative notes, anesthesia records, and post-operative care summaries. These documents ensure accurate communication of procedure specifics, complications, and recovery instructions to the receiving healthcare provider. |
| 12 | Allergy List | A patient needs to provide an updated allergy list, including specific drug, food, and environmental allergens, when requesting medical record transfers to ensure accurate and safe treatment continuity. This document should detail the type of allergic reactions experienced and any emergency interventions required to prevent adverse health outcomes. |
| 13 | Emergency Contact Information | Patients need to provide up-to-date emergency contact information, including names, phone numbers, and relationship details, to ensure timely communication in urgent situations during medical record transfers. Accurate emergency contact data is essential for healthcare providers to coordinate care and respond quickly to patient needs. |
Introduction to Medical Record Transfers
What documents does a patient need for medical record transfers? Medical record transfers require specific documentation to ensure accuracy and confidentiality during the process. Patients typically need to provide a completed medical records release form and valid identification to authorize the transfer.
Importance of Accurate Patient Documentation
Accurate patient documentation is essential for seamless medical record transfers. Proper records ensure continuity of care and prevent medical errors.
You need to provide identification documents, such as a government-issued ID, and a signed authorization form to release your medical records. These documents verify your identity and grant permission for the transfer.
Core Patient Identification Documents
Accurate medical record transfers require essential core patient identification documents to ensure proper matching and secure handling. Collecting these documents minimizes errors and facilitates seamless communication between healthcare providers.
- Government-Issued Photo ID - A valid photo identification such as a driver's license or passport confirms the patient's identity for record verification.
- Date of Birth Documentation - Official documents showing the patient's date of birth help distinguish patients with similar names during medical record matching.
- Insurance Card - The health insurance card provides crucial payer information and assists in identifying the correct medical records for transfer.
Consent Forms for Medical Record Release
Consent forms for medical record release are essential documents when transferring your medical records between healthcare providers. These forms authorize the release and ensure the confidentiality of your health information is maintained.
- Authorization Requirement - A signed consent form legally permits the disclosure of your protected health information to another party.
- Specific Details - The form must specify which records are to be released, the recipient, and the purpose of the transfer.
- Validity Period - Consent forms typically include an expiration date, limiting how long the authorization remains effective.
Ensuring the completion and accuracy of consent forms accelerates the medical record transfer process and protects your privacy.
Detailed Medical History Reports
| Document Type | Description | Importance in Medical Record Transfers |
|---|---|---|
| Detailed Medical History Reports | Comprehensive reports containing past diagnoses, treatments, surgeries, allergies, medications, and chronic conditions. These documents provide a thorough timeline of a patient's health. | Essential for ensuring continuity of care. Detailed Medical History Reports enable healthcare providers to understand previous medical events, avoid redundant tests, and tailor future treatment plans effectively. |
| Identification Documents | Government-issued ID (e.g., driver's license, passport) to verify the patient's identity. | Required to confirm the patient's identity and prevent unauthorized release of medical records. |
| Medical Release Authorization Form | Official consent form signed by the patient allowing healthcare providers to share medical records between facilities. | Legally necessary for transferring medical information to protect patient confidentiality and privacy. |
| Insurance Information | Details about the patient's health insurance provider and policy number. | Facilitates billing and verification of coverage for medical treatments. |
| Previous Test Results and Imaging | Lab reports, X-rays, MRIs, and other diagnostic images. | Provides critical data that supports accurate diagnosis and treatment planning. |
You should ensure that the Detailed Medical History Reports are accurate and up-to-date before initiating a medical record transfer to maintain the highest quality of care.
Immunization and Vaccination Records
Immunization and vaccination records are essential documents for transferring medical records. They provide a comprehensive history of the vaccines you have received, ensuring continuity of care and proper medical decisions.
To transfer your immunization records, a patient typically needs a formal request form or authorization for medical record release. The request should include personal identification details and specify the records needed. Sometimes, proof of identity or contact information for the previous healthcare provider is required to facilitate the transfer.
Current Medication and Allergy Lists
Patients must provide an up-to-date list of current medications to ensure safe and accurate medical record transfers. This list should include drug names, dosages, and administration schedules to prevent potential drug interactions. A detailed allergy list, highlighting any known drug, food, or environmental allergies, is essential to avoid adverse reactions during treatment.
Previous Surgery and Hospitalization Summaries
Patients requesting medical record transfers must provide detailed summaries of previous surgeries to ensure accurate treatment continuity. Hospitalization summaries are essential documents that outline the patient's past admissions, treatments, and outcomes. These records help healthcare providers make informed decisions and avoid medical errors during ongoing care.
Insurance and Billing Information
Medical record transfers require specific documents to ensure accurate insurance and billing processing. Proper documentation helps avoid delays and ensures coverage is correctly applied.
- Insurance Card - Provides crucial information including policy number and provider details for billing purposes.
- Authorization Form - Grants permission to release your medical records to the new healthcare provider or insurer.
- Billing Statements - Include previous invoices and payment records to verify outstanding balances and payment history.
What Documents Does a Patient Need for Medical Record Transfers? Infographic