Patients seeking a second medical opinion should bring all relevant medical records, including previous test results, imaging studies, and treatment history. It is essential to have copies of referral letters, current medications, and any lab reports to provide the consulting physician with a comprehensive understanding of the case. Proper documentation ensures an accurate evaluation and enhances the quality of the second opinion.
What Documents Does a Patient Need for a Second Medical Opinion?
| Number | Name | Description |
|---|---|---|
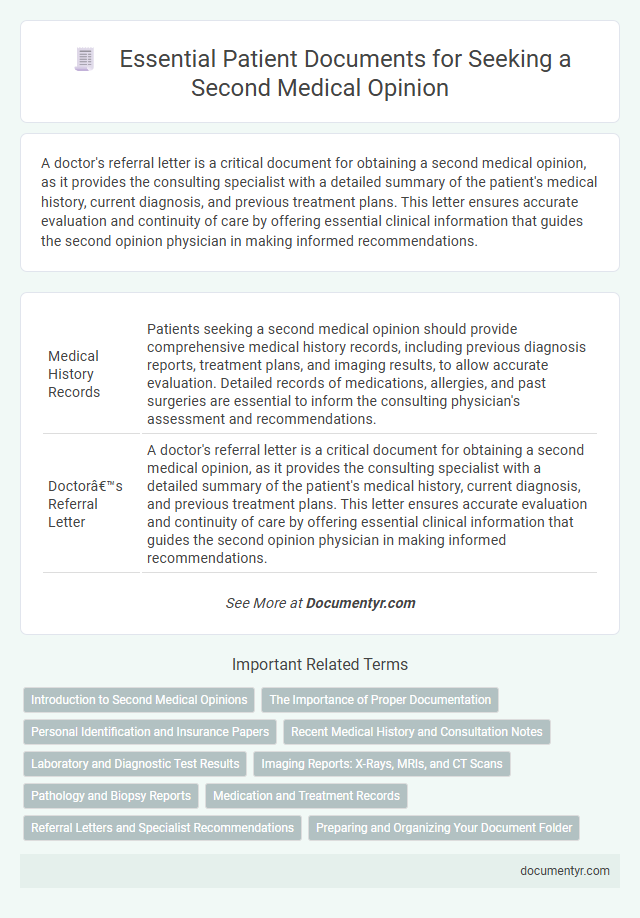
| 1 | Medical History Records | Patients seeking a second medical opinion should provide comprehensive medical history records, including previous diagnosis reports, treatment plans, and imaging results, to allow accurate evaluation. Detailed records of medications, allergies, and past surgeries are essential to inform the consulting physician's assessment and recommendations. |
| 2 | Doctor’s Referral Letter | A doctor's referral letter is a critical document for obtaining a second medical opinion, as it provides the consulting specialist with a detailed summary of the patient's medical history, current diagnosis, and previous treatment plans. This letter ensures accurate evaluation and continuity of care by offering essential clinical information that guides the second opinion physician in making informed recommendations. |
| 3 | Diagnosis Report | A patient seeking a second medical opinion should bring all relevant diagnosis reports, including laboratory results, imaging scans, and pathology findings, to provide comprehensive clinical information. These documents enable the consulting physician to accurately assess the initial diagnosis and recommend appropriate treatment options. |
| 4 | Pathology Reports | Patients seeking a second medical opinion should provide comprehensive pathology reports, including biopsy results, histopathology findings, and immunohistochemistry data, to ensure accurate diagnosis verification. Detailed laboratory analyses and imaging summaries are crucial for specialists to review tumor characteristics, disease staging, and treatment response effectively. |
| 5 | Radiology Images (X-rays, CT scans, MRI, Ultrasound) | Patients seeking a second medical opinion should provide complete radiology images such as X-rays, CT scans, MRI, and Ultrasound along with detailed radiology reports to ensure accurate assessment. High-quality digital copies or original films are essential for specialists to review anatomical details, diagnose conditions, and recommend appropriate treatment plans. |
| 6 | Radiology Reports | Patients seeking a second medical opinion should bring all relevant radiology reports, including MRI, CT scans, X-rays, and ultrasound images, to provide comprehensive diagnostic information. Detailed radiology documentation enables the consulting physician to accurately assess previous findings, compare imaging results, and recommend appropriate treatment options. |
| 7 | Laboratory Test Results | Patients seeking a second medical opinion should provide complete laboratory test results, including blood work, imaging reports, and biopsy outcomes, to ensure accurate assessment. These documents enable the consulting physician to review prior diagnostics, identify discrepancies, and recommend appropriate treatment options. |
| 8 | Biopsy Reports | Patients seeking a second medical opinion should bring comprehensive biopsy reports, including pathology findings, tissue sample analyses, and diagnostic imaging results. These documents are crucial for accurate evaluation and comparison, enabling the consulting physician to provide an informed assessment of the medical condition. |
| 9 | Surgery Reports | Surgery reports are essential documents for a patient seeking a second medical opinion as they provide detailed information about previous surgical procedures, including operative findings, techniques used, and postoperative outcomes. These reports enable the consulting physician to accurately assess the surgical history, identify potential complications, and recommend appropriate treatment alternatives. |
| 10 | Hospital Discharge Summary | A hospital discharge summary is essential for a second medical opinion as it provides a comprehensive overview of the patient's diagnosis, treatment, and hospital course. This document includes critical information such as the reason for admission, procedures performed, medications prescribed, and follow-up care instructions, enabling the consulting physician to assess the initial treatment accurately. |
| 11 | Treatment Records (Prescriptions, Medication Lists) | Patients seeking a second medical opinion should provide comprehensive treatment records, including detailed prescriptions and current medication lists, to ensure accurate evaluation and tailored recommendations. These documents enable the consulting physician to review prior treatments, assess drug interactions, and formulate an effective alternative care plan. |
| 12 | Immunization Records | Patients seeking a second medical opinion should provide comprehensive immunization records that detail all vaccines received, including dates and types, to ensure accurate assessment of their immune status. These documents assist healthcare providers in identifying potential vaccine-related factors influencing the diagnosis and treatment plan. |
| 13 | Allergy Information | Patients seeking a second medical opinion should bring comprehensive allergy information, including detailed records of any known drug, food, or environmental allergies, as well as documentation of past allergic reactions and treatments. Accurate allergy data ensures the consulting physician can safely evaluate alternative diagnostic and treatment options. |
| 14 | Consent Forms | Patients seeking a second medical opinion must provide signed consent forms authorizing the release and review of their medical records to ensure confidentiality and compliance with privacy laws. These documents enable healthcare providers to access accurate medical history, facilitating an informed and comprehensive evaluation. |
| 15 | Personal Identification (Photo ID, Insurance Card) | Patients seeking a second medical opinion must provide valid personal identification, such as a government-issued photo ID and their health insurance card, to verify identity and coverage eligibility. These documents ensure smooth communication between healthcare providers and facilitate access to medical records and insurance benefits. |
Introduction to Second Medical Opinions
A second medical opinion provides an opportunity to confirm a diagnosis, explore alternative treatments, and ensure the best possible healthcare decisions. It is a common practice for patients seeking reassurance or additional expertise on complex medical issues.
When requesting a second opinion, organizing your medical documents is essential. Your records should include imaging reports, laboratory results, physician notes, and any treatment history to provide comprehensive information to the consulting specialist.
The Importance of Proper Documentation
What documents are essential for obtaining a second medical opinion? Proper documentation ensures accurate evaluation and reduces delays in diagnosis or treatment. Your medical records, test results, and previous doctor's notes provide the foundation for a thorough review.
Personal Identification and Insurance Papers
| Document Type | Description | Importance |
|---|---|---|
| Personal Identification | Official government-issued ID such as a passport, driver's license, or national identity card. | Confirms patient identity, ensures accurate medical record matching, and facilitates secure communication between healthcare providers. |
| Insurance Papers | Health insurance card, policy details, or proof of insurance coverage. | Verifies insurance status for billing purposes and determines coverage eligibility for the requested second opinion consultation and any related procedures. |
Recent Medical History and Consultation Notes
Obtaining a second medical opinion requires thorough documentation to ensure accurate assessment. Recent medical history and consultation notes play a crucial role in providing a comprehensive overview of your health status.
- Recent Medical History - Detailed records of symptoms, diagnoses, treatments, and hospital visits within the past months aid in understanding the progression of your condition.
- Consultation Notes - Notes from previous healthcare providers include clinical observations, diagnostic test results, and treatment recommendations necessary for comparison.
- Diagnostic Reports - Lab results, imaging studies, and pathology reports complement the recent medical history and consultation notes for a complete evaluation.
Laboratory and Diagnostic Test Results
Laboratory and diagnostic test results are essential documents for obtaining a second medical opinion. These results provide detailed information about your current health status and help the consulting physician make informed decisions. Ensuring these documents are complete and accurate speeds up the review process and enhances the quality of the second opinion.
Imaging Reports: X-Rays, MRIs, and CT Scans
Imaging reports are essential documents for obtaining a second medical opinion, providing detailed insights into a patient's condition. These reports include X-rays, MRIs, and CT scans, which offer visual evidence critical for accurate diagnosis and treatment planning.
- X-Rays - X-ray images reveal bone fractures, lung conditions, and other structural issues important for evaluation.
- MRIs - MRI scans provide high-resolution images of soft tissues, brain, and spinal cord, critical for detailed assessment.
- CT Scans - CT scans offer cross-sectional views of organs and tissues, essential for detecting tumors, infections, and internal injuries.
Providing complete and clear imaging reports ensures a reliable and comprehensive second medical opinion.
Pathology and Biopsy Reports
Obtaining a second medical opinion requires comprehensive documentation to ensure accurate evaluation, especially focusing on pathology and biopsy reports. These documents provide crucial insights into the diagnosis and guide treatment options.
- Pathology Report - Contains detailed analysis of tissue samples, highlighting cellular abnormalities and disease characteristics essential for diagnosis verification.
- Biopsy Report - Summarizes the findings from tissue extraction, including type, location, and results pivotal for confirming the initial diagnosis.
- Lab Test Results - Includes relevant blood work and molecular testing that support the pathology findings and influence treatment recommendations.
Medication and Treatment Records
Patients seeking a second medical opinion should bring comprehensive medication records, including current prescriptions, dosages, and any past medications related to their condition. Detailed treatment records such as surgery reports, therapy notes, and diagnostic test results provide essential context for accurate evaluation. Providing these documents ensures the consulting physician can offer a well-informed and precise assessment.
Referral Letters and Specialist Recommendations
When seeking a second medical opinion, referral letters play a crucial role in providing comprehensive background information. These documents summarize your primary physician's findings and outline the reasons for requesting further evaluation.
Specialist recommendations offer insights into the appropriate experts to consult based on your condition. Ensuring you have both referral letters and specialist advice helps streamline the process and supports accurate diagnosis and treatment planning.
What Documents Does a Patient Need for a Second Medical Opinion? Infographic