Medical documents required for workers' compensation claims typically include detailed medical reports, treatment records, and diagnostic test results that substantiate the injury or illness. Physicians' notes describing the diagnosis, treatment plan, and prognosis are essential for validating the claim and determining compensation eligibility. Accurate and timely submission of these documents ensures proper evaluation and facilitates the claim process.
What Medical Documents are Required for Workers’ Compensation Claims?
| Number | Name | Description |
|---|---|---|
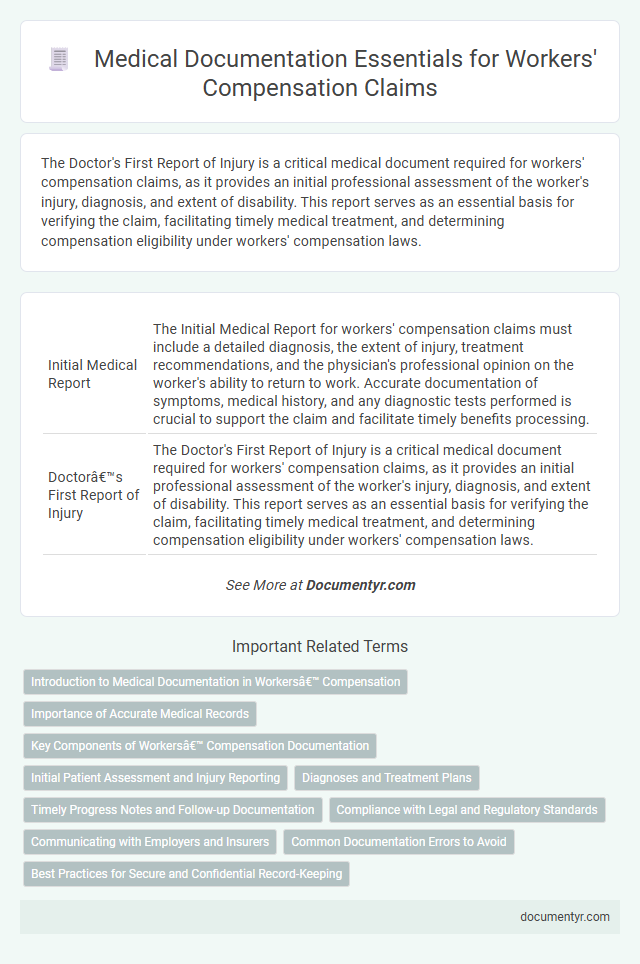
| 1 | Initial Medical Report | The Initial Medical Report for workers' compensation claims must include a detailed diagnosis, the extent of injury, treatment recommendations, and the physician's professional opinion on the worker's ability to return to work. Accurate documentation of symptoms, medical history, and any diagnostic tests performed is crucial to support the claim and facilitate timely benefits processing. |
| 2 | Doctor’s First Report of Injury | The Doctor's First Report of Injury is a critical medical document required for workers' compensation claims, as it provides an initial professional assessment of the worker's injury, diagnosis, and extent of disability. This report serves as an essential basis for verifying the claim, facilitating timely medical treatment, and determining compensation eligibility under workers' compensation laws. |
| 3 | Medical Evaluation Form | The Medical Evaluation Form is a critical document in workers' compensation claims, detailing the employee's injury diagnosis, treatment plan, and prognosis as assessed by a licensed healthcare professional. This form ensures accurate medical documentation, supporting the claim's validity and facilitating timely compensation decisions. |
| 4 | Progress Notes | Progress notes are essential medical documents in workers' compensation claims, providing detailed, chronological records of a patient's clinical status, treatment plans, and responses to therapy. These notes support the evaluation of injury severity, track recovery progress, and substantiate the necessity for ongoing medical care in legal and insurance assessments. |
| 5 | Treatment Records | Treatment records provide detailed documentation of medical evaluations, diagnoses, and therapeutic interventions essential for substantiating workers' compensation claims. Accurate and comprehensive treatment records help establish the connection between workplace injuries and required medical care, ensuring appropriate compensation and support. |
| 6 | Diagnostic Test Results (X-ray, MRI, CT scan) | Diagnostic test results such as X-rays, MRIs, and CT scans are essential medical documents for workers' compensation claims, providing objective evidence of injury severity and location. These imaging reports support injury diagnosis, guide treatment plans, and validate the claimant's medical condition for accurate compensation assessment. |
| 7 | Operative Reports | Operative reports are essential medical documents in workers' compensation claims, providing detailed accounts of surgical procedures, including the extent of injuries, techniques used, and postoperative findings. These reports serve as critical evidence to validate the necessity of treatment and support the claimant's entitlement to benefits. |
| 8 | Hospital Discharge Summaries | Hospital discharge summaries serve as crucial medical documents for workers' compensation claims, providing detailed records of treatment, diagnosis, and prognosis following hospitalization due to a work-related injury. These summaries offer precise information on the patient's condition, medical interventions, and discharge instructions, which support claim validation and facilitate appropriate compensation decisions. |
| 9 | Prescription Records | Prescription records serve as critical medical documents in workers' compensation claims, providing detailed evidence of prescribed treatments and medications related to the workplace injury. These records help verify the extent of injury, support the legitimacy of the claim, and guide appropriate medical care during the recovery process. |
| 10 | Functional Capacity Evaluation (FCE) | A Functional Capacity Evaluation (FCE) is a critical medical document required for workers' compensation claims to objectively assess an injured worker's ability to perform work-related tasks. Detailed FCE reports provide essential data on physical limitations and capabilities, helping to determine appropriate injury benefits and work restrictions. |
| 11 | Work Status Reports | Work status reports are critical medical documents in workers' compensation claims, providing detailed information about an employee's ability to perform job duties and recommended work restrictions. These reports, typically completed by healthcare providers, help determine eligibility for benefits and guide return-to-work decisions. |
| 12 | Disability Verification | Disability verification for workers' compensation claims requires comprehensive medical documentation including physician's disability evaluation reports, diagnostic test results, and treatment records confirming the employee's inability to work. Accurate and timely submission of these medical documents ensures proper assessment of disability status and eligibility for compensation benefits. |
| 13 | Independent Medical Examination (IME) Report | An Independent Medical Examination (IME) report is a critical medical document required for workers' compensation claims, providing an objective assessment of the injured worker's condition by a qualified, impartial physician. This report includes detailed findings, diagnosis, treatment recommendations, and an evaluation of the worker's ability to return to work, which directly influences claim approvals and benefit determinations. |
| 14 | Return-to-Work Release | A Return-to-Work Release, often mandated in workers' compensation claims, is a critical medical document issued by a healthcare provider confirming the employee's capacity to resume job duties either fully or with specific restrictions. This document ensures compliance with occupational health standards and facilitates a smooth transition while minimizing the risk of re-injury or prolonged disability. |
| 15 | Permanent Impairment Rating | Permanent Impairment Ratings require detailed medical evidence including physician evaluation reports, diagnostic test results, and records of functional limitations related to the injury. Documentation must align with state-specific guidelines, such as the AMA Guides to the Evaluation of Permanent Impairment, to support the claim and determine compensation eligibility. |
| 16 | Physical Therapy Reports | Physical therapy reports are essential medical documents for workers' compensation claims, providing detailed assessments of injury-related impairments and progress in rehabilitation. These reports include treatment plans, session notes, range of motion measurements, pain levels, and functional capacity evaluations critical to validating the necessity and effectiveness of prescribed therapy. |
| 17 | Specialist Consultation Reports | Specialist consultation reports are crucial medical documents for workers' compensation claims, providing detailed evaluations and expert opinions on the nature and extent of the injury or illness related to the workplace. These reports include diagnostic findings, treatment recommendations, and prognosis, directly supporting the claim's validity and guiding appropriate compensation decisions. |
| 18 | Pain Management Records | Pain management records, including detailed treatment notes, medication logs, and pain assessment scales, are critical medical documents for workers' compensation claims to substantiate the extent and impact of an injury. These records provide objective evidence of ongoing symptoms and treatment efficacy, supporting the legitimacy and severity of a claimant's pain-related conditions. |
| 19 | Medical Billing Statements | Medical billing statements are essential for workers' compensation claims as they provide detailed records of services rendered, treatment dates, and costs incurred, which validate the medical expenses related to the injury. These documents must itemize charges, include provider information, and align with the injury timeline to ensure proper reimbursement and claim approval. |
| 20 | Medical Authorization Form | A Medical Authorization Form is essential for workers' compensation claims, granting insurers permission to access medical records and verify treatment related to the workplace injury. This form ensures the timely collection of accurate documentation needed to process the claim and authorize appropriate medical benefits. |
Introduction to Medical Documentation in Workers’ Compensation
| Introduction to Medical Documentation in Workers' Compensation |
|---|
| Medical documentation is a critical component of workers' compensation claims. Accurate and comprehensive medical records establish the extent of the injury or illness and support the claim process. Your medical documents must clearly reflect diagnosis, treatment plans, and any work restrictions prescribed by healthcare providers. Commonly required medical documents include initial medical reports, diagnostic test results, treatment summaries, and physician's statements. Proper medical documentation helps ensure timely claim approvals and appropriate compensation for work-related injuries or illnesses. |
Importance of Accurate Medical Records
Accurate medical records are crucial for workers' compensation claims as they provide detailed evidence of your injury and treatment. These documents help establish the legitimacy and extent of the work-related injury or illness.
Medical records required typically include initial injury reports, physician's notes, diagnostic test results, and treatment plans. Precise documentation ensures the claims process proceeds smoothly and supports fair compensation. Maintaining thorough and accurate records can significantly impact the outcome of your workers' compensation case.
Key Components of Workers’ Compensation Documentation
Medical documents play a crucial role in validating workers' compensation claims by providing evidence of injury and treatment. Proper documentation ensures accurate assessment and timely processing of claims.
- Incident Report - Detailed account of the workplace injury, including date, time, and circumstances, establishing the claim's basis.
- Medical Records - Comprehensive records from healthcare providers documenting diagnosis, treatment plans, and prognosis related to the injury.
- Physician's Evaluation - Professional assessment detailing the extent of injury, ability to work, and recommended medical care.
- Return-to-Work Status - Documentation indicating the worker's capacity to resume job duties or any restrictions necessary for recovery.
- Billing and Payment Records - Invoices and receipts for medical services and treatments that verify expenses covered under workers' compensation.
Initial Patient Assessment and Injury Reporting
Initial patient assessment documents are crucial for workers' compensation claims as they provide detailed information on the injury and the patient's medical condition. Comprehensive injury reports must include the date, location, and cause of the injury along with the symptoms observed during the first examination. Your submission should consist of medical evaluations, treatment plans, and any diagnostic test results to ensure accurate processing and validation of the claim.
Diagnoses and Treatment Plans
Medical documents play a crucial role in supporting workers' compensation claims, particularly those related to diagnoses and treatment plans. Accurate and thorough documentation ensures that your claim is properly evaluated and approved.
- Medical Diagnoses - Detailed diagnosis reports from licensed healthcare professionals confirm the specific injury or illness linked to the workplace incident.
- Treatment Plans - Comprehensive treatment plans outline the prescribed medical care, including medications, therapies, and recommended procedures necessary for recovery.
- Progress Notes - Regular progress notes document the patient's response to treatment, changes in condition, and ongoing medical recommendations supporting the claim's validity.
Timely Progress Notes and Follow-up Documentation
Timely progress notes are essential for workers' compensation claims as they provide a detailed record of the patient's condition and treatment over time. These notes must be accurately dated and document all medical evaluations, therapies, and patient responses to ensure compliance with legal requirements. Follow-up documentation supports the ongoing assessment of recovery and justifies continued care or modifications in treatment plans.
Compliance with Legal and Regulatory Standards
What medical documents are required for workers' compensation claims to ensure compliance with legal and regulatory standards?
Accurate medical records such as initial injury reports, physician's evaluations, and treatment plans are essential for validating injury claims. Proper documentation helps meet state-specific workers' compensation laws and supports timely claim processing by insurers and employers.
Communicating with Employers and Insurers
Medical documentation is essential for workers' compensation claims to verify injury and treatment. Clear communication with employers and insurers ensures accurate and timely claim processing.
- Medical Reports - Detailed physician evaluations outlining diagnosis, treatment, and prognosis.
- Diagnostic Tests - Laboratory results, imaging studies, and other tests supporting injury verification.
- Treatment Records - Documentation of all medical interventions, prescriptions, and therapy sessions related to the workplace injury.
You should provide complete and organized medical documents to facilitate smooth communication with your employer and the insurance company.
Common Documentation Errors to Avoid
Workers' compensation claims require accurate and complete medical documentation to ensure timely processing and appropriate benefits. Essential documents include initial injury reports, medical evaluations, treatment records, and physicians' notes.
Common documentation errors include incomplete injury descriptions, missing signatures, and unclear medical terminology. Avoid these mistakes by maintaining detailed, legible, and consistently updated medical files throughout the claim process.
What Medical Documents are Required for Workers’ Compensation Claims? Infographic