Essential documents for filing a medical malpractice claim include medical records, billing statements, and expert medical opinions that demonstrate negligence. Patient consent forms, detailed incident reports, and correspondence with healthcare providers also play a crucial role in substantiating the claim. Accurate documentation of injuries, treatment timelines, and communication with medical staff ensures a stronger legal case.
What Documents are Necessary for Medical Malpractice Claim Filing?
| Number | Name | Description |
|---|---|---|
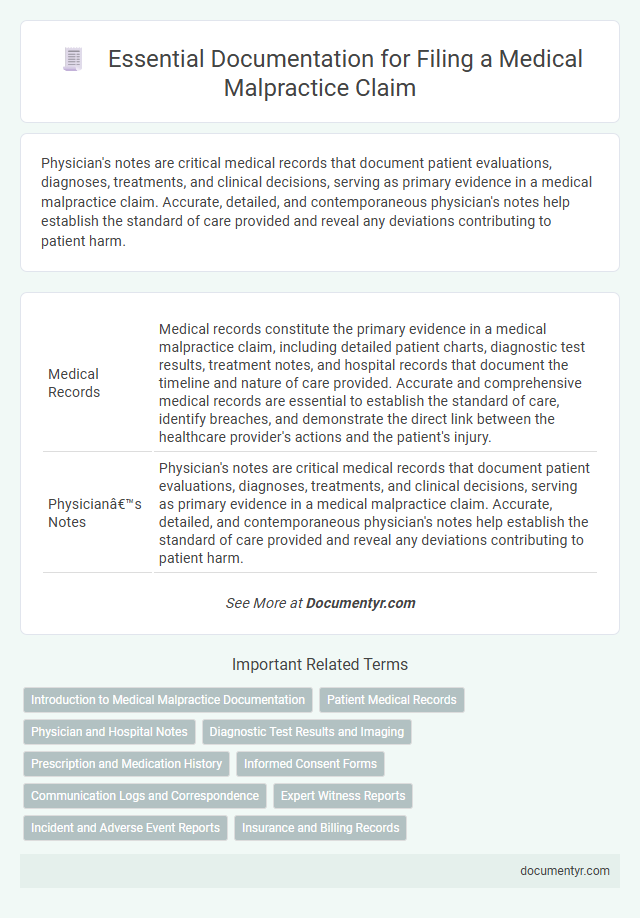
| 1 | Medical Records | Medical records constitute the primary evidence in a medical malpractice claim, including detailed patient charts, diagnostic test results, treatment notes, and hospital records that document the timeline and nature of care provided. Accurate and comprehensive medical records are essential to establish the standard of care, identify breaches, and demonstrate the direct link between the healthcare provider's actions and the patient's injury. |
| 2 | Physician’s Notes | Physician's notes are critical medical records that document patient evaluations, diagnoses, treatments, and clinical decisions, serving as primary evidence in a medical malpractice claim. Accurate, detailed, and contemporaneous physician's notes help establish the standard of care provided and reveal any deviations contributing to patient harm. |
| 3 | Hospital Admission and Discharge Summaries | Hospital admission and discharge summaries are critical documents for medical malpractice claim filing as they provide detailed records of the patient's initial condition, treatment plan, and clinical status upon discharge. These summaries offer essential evidence of the standard of care provided and any deviations that may support claims of negligence or malpractice. |
| 4 | Prescription Records | Prescription records provide critical evidence in medical malpractice claims by documenting all medications prescribed, dosages, and administration timelines, which helps establish deviations from standard care. These records enable attorneys and medical experts to identify prescription errors, adverse drug interactions, or negligent omissions that may have contributed to patient harm. |
| 5 | Diagnostic Test Results (e.g., X-rays, MRI, CT scans) | Diagnostic test results, such as X-rays, MRI, and CT scans, are crucial documents for a medical malpractice claim as they provide objective evidence of the patient's condition and potential misdiagnosis or delayed diagnosis. These medical imaging records help establish the standard of care, demonstrate any deviations by healthcare providers, and support expert testimony during the legal process. |
| 6 | Operative Reports | Operative reports are essential documents in medical malpractice claim filings as they provide detailed accounts of surgical procedures, including preoperative diagnoses, intraoperative findings, and postoperative care. These reports serve as critical evidence to establish the standard of care and identify any deviations during the operation that may have contributed to patient injury. |
| 7 | Pathology Reports | Pathology reports are essential documents in medical malpractice claim filings as they provide detailed analysis of tissue samples, confirming diagnoses or identifying errors in medical treatment. These reports serve as critical evidence to establish the standard of care breach and causation linking medical negligence to patient harm. |
| 8 | Billing and Invoices | Essential documents for medical malpractice claim filing include detailed billing statements and invoices that itemize all medical services, treatments, and associated costs. Accurate, comprehensive billing records provide critical evidence of the financial impact and support the establishment of damages during claim evaluation. |
| 9 | Insurance Claim Forms | Insurance claim forms are essential documents required for medical malpractice claim filing, providing detailed information about the claimant, healthcare provider, and incident specifics. These forms facilitate the formal submission of claims to medical malpractice insurance carriers, ensuring accurate assessment and processing of compensation requests. |
| 10 | Referral Documents | Referral documents are essential in a medical malpractice claim as they provide detailed records of the patient's initial medical evaluation and specialist consultations. These documents establish the timeline, highlight any deviations from standard care, and serve as critical evidence to support negligence or misdiagnosis claims. |
| 11 | Consent Forms | Consent forms are essential documents in medical malpractice claim filings as they verify that the patient was informed about and agreed to the medical procedures performed. These forms help establish whether proper disclosure of risks and alternatives occurred, which is critical in determining liability in malpractice cases. |
| 12 | Witness Statements | Witness statements play a crucial role in medical malpractice claim filing by providing detailed accounts of the incident from individuals who observed the medical treatment or its aftermath. These statements help establish negligence and causation, supporting the claimant's case alongside medical records, expert testimony, and relevant correspondence. |
| 13 | Expert Medical Opinions | Expert medical opinions are crucial for substantiating medical malpractice claims, typically requiring detailed reports from board-certified physicians specializing in the relevant field of medicine. These documents must clearly outline deviations from the accepted standard of care, causation of injury, and the extent of damages sustained by the patient. |
| 14 | Photographs or Imaging Evidence | Photographs and imaging evidence, such as X-rays, MRIs, and CT scans, are crucial for substantiating medical malpractice claims by visually demonstrating the extent of injuries or misdiagnosis. Properly documented and time-stamped images provide objective proof that supports patient testimonies and expert medical opinions during legal proceedings. |
| 15 | Incident or Accident Reports | Incident or accident reports are critical documents required for filing a medical malpractice claim as they provide an official record of the event, detailing the circumstances, time, location, and individuals involved. These reports serve as foundational evidence to establish the occurrence of the alleged negligence or error, supporting the claimant's case during legal proceedings. |
| 16 | Chronology of Medical Care | A detailed chronology of medical care is essential for medical malpractice claim filing, including all medical records, physician notes, diagnostic test results, treatment timelines, and correspondence between healthcare providers. This timeline helps establish the sequence of events, identify deviations from standard care, and support causation and damages claims. |
| 17 | Death Certificate (if applicable) | A certified death certificate is a crucial document in medical malpractice claim filing when the patient has died, serving as official proof of death and establishing the basis for wrongful death claims. This document must be accompanied by medical records, expert witness statements, and any relevant hospital or treatment documentation to substantiate the claim. |
| 18 | Autopsy Report (if applicable) | The autopsy report is a critical document in a medical malpractice claim, providing detailed findings on the cause and manner of death that can directly link medical errors to the fatality. This report, typically prepared by a forensic pathologist, includes histological analyses, toxicology results, and anatomical observations essential for establishing negligence or medical mismanagement. |
| 19 | Correspondence with Healthcare Providers | Detailed correspondence with healthcare providers, including emails, letters, and appointment records, is essential for substantiating a medical malpractice claim by documenting communication, treatment decisions, and potential negligence. These documents provide crucial evidence of the standard of care and the timeline of patient interactions, aiding legal evaluation and case preparation. |
| 20 | Complaint or Grievance Letters | Complaint or grievance letters are essential documents for medical malpractice claim filing as they detail the plaintiff's allegations, describe the incident, and formally express dissatisfaction with the medical provider's conduct. These letters often include dates, treatment specifics, involved medical personnel, and the harm suffered, serving as a foundational record for legal proceedings and facilitating early dispute resolution. |
Introduction to Medical Malpractice Documentation
Filing a medical malpractice claim requires precise and comprehensive documentation to support the case. Proper records establish the foundation for proving negligence and medical errors.
- Medical Records - Detailed patient charts, diagnostic reports, and treatment plans document the standard of care and any deviations.
- Expert Medical Opinions - Statements from qualified healthcare professionals assess whether the care provided met accepted medical standards.
- Consent Forms and Communication Logs - Records of patient consent and communication with healthcare providers highlight informed consent and potential miscommunication issues.
Accurate and complete documentation is critical for the successful filing and evaluation of a medical malpractice claim.
Patient Medical Records
Patient medical records are essential documents for filing a medical malpractice claim. These records contain detailed information about the patient's diagnosis, treatment, and care provided by healthcare professionals.
Accurate and complete medical records help establish the standard of care and identify any deviations that may have led to the injury. These documents include hospital charts, physician notes, test results, and prescription details critical to building a strong malpractice case.
Physician and Hospital Notes
Physician and hospital notes are essential documents for filing a medical malpractice claim. These records provide detailed accounts of the patient's medical history, treatment plans, and clinical observations. Accurate and comprehensive notes help establish the standard of care and demonstrate any deviations that may indicate negligence.
Diagnostic Test Results and Imaging
Submitting a medical malpractice claim requires careful documentation to support your case effectively. Diagnostic test results and imaging play a critical role in demonstrating errors or omissions in medical care.
- Diagnostic Test Results - Include laboratory reports such as blood tests, pathology, and biopsy results that reveal abnormal findings or misinterpretations.
- Imaging Records - Obtain X-rays, MRIs, CT scans, and ultrasounds that show physical evidence of injury or misdiagnosis relevant to your claim.
- Official Medical Reports - Secure detailed radiologist and specialist interpretations that provide professional insights correlating with the diagnostic data.
Prescription and Medication History
What prescription and medication history documents are necessary for filing a medical malpractice claim? Detailed records of all prescribed medications, including dosages and administration dates, are essential to establish the treatment timeline. Pharmacy records and doctor's prescription notes provide critical evidence to support the claim.
Informed Consent Forms
Informed consent forms are crucial documents in medical malpractice claim filing. They provide evidence that the patient was made aware of potential risks before treatment.
- Definition - Informed consent forms confirm that a patient voluntarily agreed to a medical procedure after understanding its risks and benefits.
- Importance - These forms demonstrate whether the healthcare provider adequately communicated potential complications or alternatives to the patient.
- Legal Relevance - Properly signed informed consent forms can influence the outcome of a malpractice case by establishing patient awareness and consent.
Communication Logs and Correspondence
Communication logs and correspondence are critical documents for filing a medical malpractice claim, as they provide detailed records of interactions between you and healthcare providers. These documents include emails, letters, appointment notes, and phone call records that help establish timelines and verify reported information. Maintaining thorough communication records supports the accuracy and credibility of your malpractice claim throughout the legal process.
Expert Witness Reports
Expert witness reports play a crucial role in medical malpractice claim filing. These documents provide professional evaluations that support the validity of your case.
Expert reports typically include detailed analyses from qualified medical professionals who review the facts and determine whether the standard of care was breached. These reports must be thorough, clearly stating how the alleged negligence caused harm. Securing credible expert testimony strengthens the evidence needed for successful litigation.
Incident and Adverse Event Reports
Incident and adverse event reports are critical documents for medical malpractice claim filing. These reports provide detailed accounts of the medical error or negligence that led to patient harm.
Hospitals and healthcare providers generate these reports immediately after an adverse event occurs. Your attorney will use them to establish the facts and support your claim effectively.
What Documents are Necessary for Medical Malpractice Claim Filing? Infographic