Essential documents for a second medical opinion include the patient's complete medical history, recent test results such as blood work and imaging scans, and all relevant treatment records. Providing detailed notes on current symptoms and previous diagnoses helps specialists offer accurate insights. Copies of prior consultation summaries and medication lists also ensure a comprehensive evaluation.
What Documents are Necessary for a Second Medical Opinion?
| Number | Name | Description |
|---|---|---|
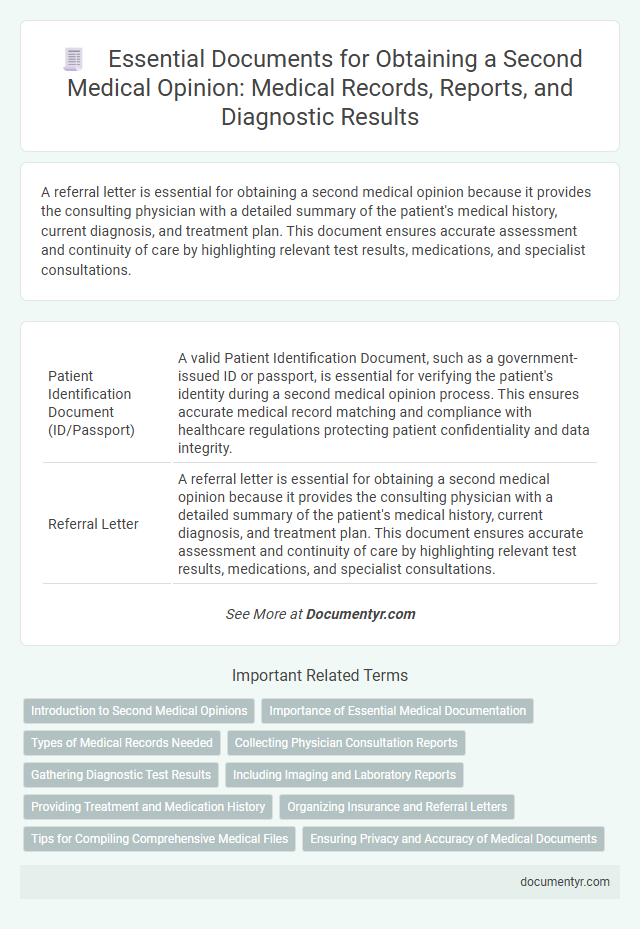
| 1 | Patient Identification Document (ID/Passport) | A valid Patient Identification Document, such as a government-issued ID or passport, is essential for verifying the patient's identity during a second medical opinion process. This ensures accurate medical record matching and compliance with healthcare regulations protecting patient confidentiality and data integrity. |
| 2 | Referral Letter | A referral letter is essential for obtaining a second medical opinion because it provides the consulting physician with a detailed summary of the patient's medical history, current diagnosis, and treatment plan. This document ensures accurate assessment and continuity of care by highlighting relevant test results, medications, and specialist consultations. |
| 3 | Primary Physician Report | The primary physician report is essential for a second medical opinion as it contains the initial diagnosis, treatment plan, and clinical findings crucial for accurate evaluation. This document provides the specialist with comprehensive patient history and diagnostic test results, enabling informed recommendations. |
| 4 | Medical History Summary | A comprehensive Medical History Summary is essential for a second medical opinion, including detailed records of past diagnoses, treatments, surgical procedures, allergies, and medications. Accurate and up-to-date documentation ensures the consulting physician can thoroughly evaluate your condition and provide precise recommendations. |
| 5 | Previous Consultation Records | Previous consultation records, including detailed reports, diagnostic test results, imaging studies, and treatment summaries, are essential documents for obtaining a second medical opinion. These records provide the consulting physician with comprehensive insights into the patient's medical history and initial diagnosis, enabling a more accurate and informed evaluation. |
| 6 | Hospital Discharge Summary | A Hospital Discharge Summary is crucial for obtaining a second medical opinion as it provides a comprehensive overview of the patient's diagnosis, treatment, hospital course, and recommendations for follow-up care. This document allows the consulting physician to review the initial medical evaluation, identify any discrepancies, and formulate an informed, alternative treatment plan based on the patient's recent clinical history. |
| 7 | Laboratory Test Results | Laboratory test results such as blood work, imaging reports, biopsy analyses, and pathology findings are essential documents for obtaining a second medical opinion. These detailed records provide critical insights into the patient's health status and enable the consulting physician to make an accurate and informed assessment. |
| 8 | Imaging Reports (X-ray, CT, MRI, Ultrasound) | Imaging reports such as X-rays, CT scans, MRIs, and ultrasounds are essential documents for obtaining a second medical opinion, as they provide critical visual evidence of anatomical and pathological conditions. Including detailed radiology reports along with the corresponding images ensures accurate assessment and informed recommendations by the consulting physician. |
| 9 | Pathology Reports/Biopsy Results | Pathology reports and biopsy results are essential documents for obtaining a second medical opinion, providing detailed analysis of tissue samples to confirm or clarify a diagnosis. These reports include microscopic findings, diagnostic conclusions, and immunohistochemical test results, enabling the consulting physician to accurately assess the medical condition and recommend appropriate treatment options. |
| 10 | Surgical Reports/Operative Notes | Surgical reports or operative notes are essential documents for obtaining a second medical opinion as they provide detailed descriptions of the procedures performed, including surgical techniques, findings, and any complications encountered. These records enable the consulting physician to thoroughly evaluate the initial treatment and recommend alternative approaches or confirm the existing plan with greater accuracy. |
| 11 | Medication List | A detailed medication list, including dosages and duration, is essential for obtaining an accurate second medical opinion, as it helps the reviewing physician assess potential drug interactions and treatment effectiveness. Comprehensive records of current and past medications support informed diagnostic decisions and tailored therapeutic recommendations. |
| 12 | Allergy List | An allergy list, including specific allergens and reaction details, is essential for a second medical opinion to accurately assess potential risks and tailor treatment options. Providing up-to-date immunization records and previous diagnostic test results can further support a comprehensive evaluation by the consulting physician. |
| 13 | Immunization Records | Immunization records are essential for a second medical opinion as they provide detailed information about past vaccinations, supporting accurate assessment of immunological history and potential contraindications. Including complete and up-to-date immunization documentation helps healthcare providers evaluate vaccine-related concerns and tailor treatment recommendations effectively. |
| 14 | Treatment Plans | Essential documents for obtaining a second medical opinion on treatment plans include the patient's complete medical records, detailed treatment history, diagnostic test results, imaging reports, and any current or past medication lists. Providing these comprehensive documents ensures accurate evaluation and tailored recommendations from the consulting specialist. |
| 15 | Progress Notes | Progress notes are essential documents for a second medical opinion, as they provide a detailed and chronological record of the patient's clinical status, treatments, and responses. These notes help the consulting physician understand the patient's medical history, current condition, and ongoing care plan to offer accurate and informed recommendations. |
| 16 | Specialist Opinions (if any) | Specialist opinions require comprehensive medical records including previous diagnoses, imaging studies such as MRIs or X-rays, lab test results, and detailed treatment histories to facilitate accurate reassessment. Providing referral letters and documented symptom progression enhances the specialist's ability to deliver a precise and informed second medical opinion. |
| 17 | Consent Forms | Consent forms are essential documents for obtaining a second medical opinion, ensuring that the patient authorizes the sharing of their medical records and personal health information with the consulting physician. These forms protect patient privacy under HIPAA regulations and facilitate accurate review and diagnosis by the second medical provider. |
| 18 | Insurance Information/Authorization | For a second medical opinion, it is essential to provide insurance information and authorization documents to ensure coverage and approval from the insurance provider. These documents typically include your insurance policy number, pre-authorization forms, and any referral letters required by your insurance company. |
| 19 | Recent Vital Signs Chart | Recent vital signs charts, including blood pressure, heart rate, temperature, respiratory rate, and oxygen saturation levels, are essential documents required for a comprehensive second medical opinion. These charts provide crucial real-time clinical data that enable specialists to assess the patient's current health status accurately and determine any necessary adjustments in diagnosis or treatment. |
| 20 | Rehabilitation/Therapy Reports | Rehabilitation and therapy reports are essential documents for a second medical opinion, providing detailed information on treatment progress, functional improvements, and response to interventions. These reports include physical therapy notes, occupational therapy evaluations, and progress summaries that help specialists assess ongoing care and recommend optimized rehabilitation strategies. |
Introduction to Second Medical Opinions
| Introduction to Second Medical Opinions | |
|---|---|
| Purpose | Obtain confirmation or alternative perspectives on diagnosis, treatment options, or prognosis. |
| Importance of Documentation | Essential for accurate evaluation and effective assessment by another healthcare professional. |
| Necessary Documents | Comprehensive medical records, including previous diagnoses, lab results, imaging reports, pathology slides, and treatment summaries. |
| Role of Patient | You play a critical role in gathering and providing these documents to ensure a thorough second opinion process. |
| Benefits | Improves decision-making, increases confidence in treatment plans, and may identify additional options. |
Importance of Essential Medical Documentation
Obtaining a second medical opinion requires access to comprehensive and accurate medical documents to ensure an informed evaluation. Essential medical documentation provides the foundation for a thorough review of diagnosis and treatment options.
- Medical History Records - Detailed patient history helps specialists understand past conditions and treatments, guiding a more precise second opinion.
- Diagnostic Test Results - Laboratory tests, imaging reports, and biopsy results offer critical data for confirming or reconsidering initial diagnoses.
- Treatment Summaries - Documentation of prior treatments and medications allows the consulting physician to assess effectiveness and suggest alternatives.
Types of Medical Records Needed
When seeking a second medical opinion, it is essential to provide comprehensive medical records to ensure an accurate assessment. Key documents include diagnostic test results such as MRI scans, X-rays, and blood work reports.
Detailed physician notes and treatment history help the consulting doctor understand the patient's condition and progression. Copies of surgical reports and pathology findings are also critical for a thorough review.
Collecting Physician Consultation Reports
What documents are necessary for a second medical opinion? Collecting physician consultation reports is essential to provide an accurate and comprehensive understanding of your medical condition. These reports include diagnosis details, treatment plans, and test results that inform the second physician's assessment.
Gathering Diagnostic Test Results
Gathering diagnostic test results is crucial when seeking a second medical opinion to ensure an accurate and comprehensive review. Your medical history and previous examinations help specialists provide informed recommendations.
- Lab Reports - Include blood tests, urine tests, and biopsy results to give detailed insights into your current health status.
- Imaging Studies - Submit X-rays, MRIs, CT scans, and ultrasounds to allow specialists to analyze physical conditions and abnormalities.
- Pathology Reports - Provide tissue analysis outcomes that are essential for diagnosing diseases and guiding treatment options.
Including Imaging and Laboratory Reports
For a second medical opinion, it is essential to provide comprehensive medical records, including detailed imaging reports such as X-rays, MRIs, and CT scans. Laboratory reports showing blood tests, biopsy results, and other relevant diagnostic data support accurate assessment. You should also include the initial diagnosis and treatment plans to ensure the consulting physician has a complete understanding of your medical history.
Providing Treatment and Medication History
Providing your complete treatment and medication history is essential when seeking a second medical opinion. Accurate documentation helps specialists understand your condition and previous interventions.
Necessary documents include detailed records of past treatments, prescribed medications, dosage, and duration. Lab results, imaging studies, and surgical reports contribute critical insights. You should also include any notes on side effects or complications experienced during prior therapies.
Organizing Insurance and Referral Letters
Obtaining a second medical opinion requires careful organization of essential documents to ensure a smooth review process. Key documents include insurance information and referral letters from your primary healthcare provider.
Insurance documents confirm your coverage and facilitate billing between medical providers. Referral letters provide detailed medical history and justify the need for a second evaluation, helping specialists understand your case quickly.
Tips for Compiling Comprehensive Medical Files
Gathering complete medical records is crucial for obtaining an accurate second medical opinion. Essential documents include previous test results, imaging reports, treatment histories, and physician notes. Organize these files chronologically to facilitate a clear understanding of the patient's medical journey.
What Documents are Necessary for a Second Medical Opinion? Infographic