To obtain reimbursement for durable medical equipment (DME), patients must provide a valid prescription from a licensed healthcare provider specifying the type of equipment needed. Documentation should include detailed medical records supporting the necessity of the equipment, along with a completed DME claim form submitted to the insurance provider. Proof of purchase or rental receipts is also essential to ensure proper evaluation and processing of the reimbursement request.
What Documents are Needed for Durable Medical Equipment Reimbursement?
| Number | Name | Description |
|---|---|---|
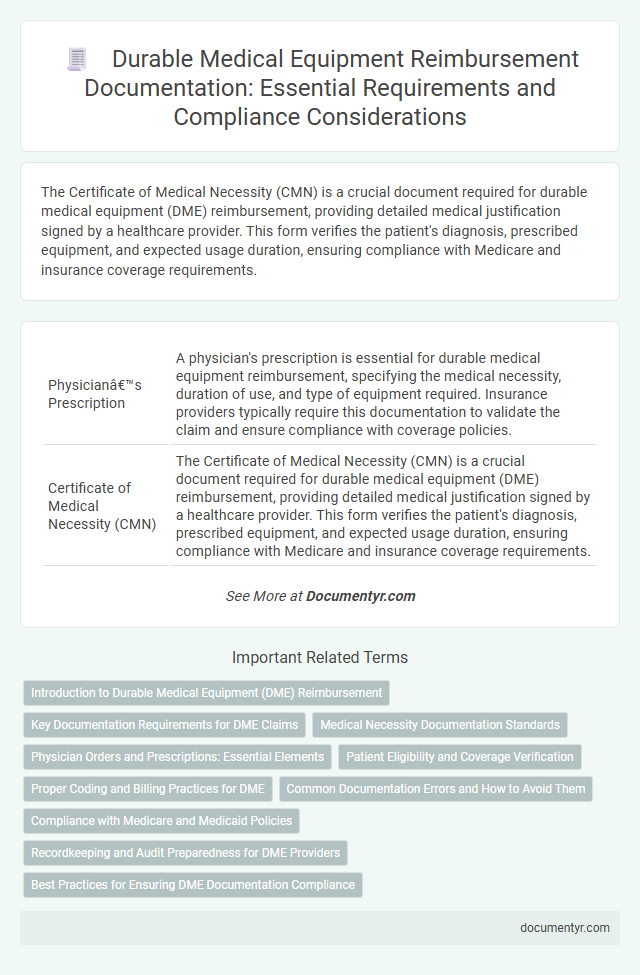
| 1 | Physician’s Prescription | A physician's prescription is essential for durable medical equipment reimbursement, specifying the medical necessity, duration of use, and type of equipment required. Insurance providers typically require this documentation to validate the claim and ensure compliance with coverage policies. |
| 2 | Certificate of Medical Necessity (CMN) | The Certificate of Medical Necessity (CMN) is a crucial document required for durable medical equipment (DME) reimbursement, providing detailed medical justification signed by a healthcare provider. This form verifies the patient's diagnosis, prescribed equipment, and expected usage duration, ensuring compliance with Medicare and insurance coverage requirements. |
| 3 | Detailed Written Order (DWO) | A Detailed Written Order (DWO) is essential for durable medical equipment reimbursement, specifying the patient's diagnosis, prescribed item, and medical necessity. This document must be signed and dated by the prescribing healthcare provider to comply with Medicare and insurance requirements. |
| 4 | Proof of Medical Diagnosis | Proof of medical diagnosis must include detailed documentation from a licensed healthcare provider specifying the patient's condition and the necessity of durable medical equipment (DME) for treatment. Essential documents typically consist of a physician's prescription, clinical notes, diagnostic test results, and any relevant medical history confirming the diagnosis to support reimbursement claims. |
| 5 | Patient Medical Records | Patient medical records must include detailed physician prescriptions, diagnostic reports, and treatment plans to validate the necessity of durable medical equipment (DME) for reimbursement claims. Documentation should clearly demonstrate the patient's medical condition, prescribed equipment specifications, and duration of use to meet payer requirements. |
| 6 | Insurance Authorization/Pre-authorization Letter | Insurance authorization or pre-authorization letters are essential documents required for durable medical equipment (DME) reimbursement, as they confirm the insurance provider's approval for the prescribed equipment. These letters must detail the patient's diagnosis, prescribed DME, medical necessity, and duration of use to ensure compliance with insurance policies and facilitate timely claim processing. |
| 7 | Durable Medical Equipment Supplier Invoice | Durable Medical Equipment reimbursement requires a detailed supplier invoice that includes the patient's information, equipment description, date of purchase, cost, and supplier credentials. Accurate documentation on the invoice ensures compliance with insurance policies and facilitates prompt claims processing. |
| 8 | Explanation of Benefits (EOB) | Explanation of Benefits (EOB) documents clearly outline the services covered, patient responsibility, and provider charges, making them essential for Durable Medical Equipment (DME) reimbursement claims. Submitting a detailed EOB along with the original DME invoice ensures accurate processing and verification by insurance companies. |
| 9 | Patient Identification (ID) | Accurate patient identification is essential for durable medical equipment (DME) reimbursement and requires documents such as a government-issued photo ID or insurance card verifying the patient's identity and eligibility. Medical providers must ensure that patient information matches across all documentation to prevent claim denials and facilitate smoother processing. |
| 10 | Assignment of Benefits Form | The Assignment of Benefits Form is essential for durable medical equipment reimbursement as it authorizes the healthcare provider to receive payments directly from the insurance company. This form, alongside the physician's prescription and detailed invoice, ensures a streamlined claims process and timely reimbursement for eligible medical equipment. |
| 11 | Delivery/Proof of Delivery Receipt | A Delivery or Proof of Delivery Receipt is essential for durable medical equipment reimbursement, serving as official evidence that the patient received the prescribed device. This document typically includes the date of delivery, patient's name, equipment details, and recipient's signature, ensuring compliance with insurance provider requirements. |
| 12 | Prior Authorization Approval Letter | The prior authorization approval letter is essential for durable medical equipment (DME) reimbursement as it verifies that the medical necessity has been reviewed and approved by the insurer. This document must include patient details, prescribed equipment specifics, approval dates, and authorization numbers to ensure smooth and timely claim processing. |
| 13 | DME Supplier Accreditation Certificate | The Durable Medical Equipment (DME) Supplier Accreditation Certificate is essential for reimbursement claims, as it verifies the supplier's compliance with Medicare standards and ensures quality service. This certificate must be included with the supplier's documentation to facilitate approval and secure payment from insurers or government healthcare programs. |
| 14 | Medicare/Medicaid Card Copy (if applicable) | A copy of the Medicare or Medicaid card is essential for durable medical equipment reimbursement to verify patient eligibility and coverage details. This documentation ensures accurate processing of claims and compliance with federal healthcare guidelines. |
| 15 | Referral Letter from Healthcare Provider | A referral letter from a healthcare provider is essential for durable medical equipment (DME) reimbursement, as it verifies medical necessity and specifies the type of equipment required. This document must detail the patient's diagnosis, treatment plan, and justify how the DME supports patient care to ensure approval from insurance providers or Medicare. |
Introduction to Durable Medical Equipment (DME) Reimbursement
Durable Medical Equipment (DME) includes essential medical devices prescribed for home use, such as wheelchairs, oxygen equipment, and hospital beds. Proper documentation is crucial to ensure reimbursement from insurance providers or government programs.
To receive reimbursement, you must submit medical justification, a valid prescription, and proof of purchase along with the DME claim. Understanding the required documents streamlines the approval process and reduces claim denials.
Key Documentation Requirements for DME Claims
To secure reimbursement for Durable Medical Equipment (DME), essential documentation includes a detailed physician's prescription specifying the type of equipment and medical necessity. Supporting documents must comprise proof of delivery and the supplier's invoice itemizing the equipment provided. Medical records demonstrating ongoing patient need often bolster claims during the review process, ensuring compliance with payer requirements.
Medical Necessity Documentation Standards
| Document Type | Purpose | Details |
|---|---|---|
| Prescription or Order from a Healthcare Provider | Proves medical necessity | Must include diagnosis, prescribed equipment, date, provider's signature, and contact information |
| Detailed Medical Records | Supports claim with clinical evidence | Document patient's condition, treatment history, functional limitations, and reason for equipment |
| Face-to-Face Encounter Documentation | Confirms evaluation and recommendation | Provider's notes from a personal examination within 6 months prior to equipment order |
| Certificate of Medical Necessity (CMN) | Standardized form required by many payers | Includes patient info, equipment details, medical rationale, and provider verification |
| Supplier Documentation | Confirms equipment delivery and setup | Proof of receipt signed by patient or caregiver, description of equipment provided |
Your Durable Medical Equipment reimbursement depends on meeting strict medical necessity documentation standards set by insurers. Proper and thorough documentation ensures compliance and increases the likelihood of successful claims.
Physician Orders and Prescriptions: Essential Elements
Physician orders and prescriptions are critical documents required for durable medical equipment (DME) reimbursement. These papers confirm your medical necessity and provide details about the specific equipment prescribed.
Essential elements include the patient's diagnosis, detailed description of the equipment, and the physician's signature and date. Accurate and complete physician documentation ensures compliance with insurance policies and facilitates timely reimbursement.
Patient Eligibility and Coverage Verification
Patient eligibility and coverage verification are critical steps in the reimbursement process for Durable Medical Equipment (DME). Proper documentation ensures compliance with insurance requirements and facilitates timely claim approval.
- Patient Eligibility Verification - Confirm the patient's insurance plan covers the specific DME items based on medical necessity and policy guidelines.
- Insurance Coverage Documents - Provide current insurance card copies and pre-authorization forms as proof of coverage and approval.
- Physician's Prescription - Include a detailed prescription or order from a licensed healthcare provider specifying the DME required and its medical necessity.
Proper Coding and Billing Practices for DME
What documents are needed for durable medical equipment (DME) reimbursement? Proper documentation includes a detailed physician's prescription specifying the medical necessity of the equipment. Accurate coding using HCPCS and ICD-10 codes ensures compliance with billing standards and facilitates timely reimbursement.
How important is proper coding and billing in DME reimbursement? Correct use of HCPCS Level II codes for DME items and adherence to CPT guidelines reduce claim denials. Supporting medical records and proof of delivery must align with coding to substantiate the claim.
Common Documentation Errors and How to Avoid Them
Durable Medical Equipment (DME) reimbursement requires precise documentation to ensure claims are processed efficiently. Missing or incorrect paperwork frequently leads to denied or delayed reimbursements.
- Detailed Prescription - A physician's valid prescription specifying the exact DME item and medical necessity is essential to validate the claim.
- Proof of Medical Necessity - Comprehensive documentation such as patient diagnosis, treatment plan, and rationale must be included to substantiate the need for the equipment.
- Accurate Supplier Information - Supplier credentials and billing details must be clear and consistent to prevent administrative errors and claim rejection.
Ensuring all required documents are complete and error-free helps avoid common pitfalls in durable medical equipment reimbursement.
Compliance with Medicare and Medicaid Policies
Proper documentation is essential for durable medical equipment (DME) reimbursement to ensure compliance with Medicare and Medicaid policies. Accurate records support claims and protect against audits and denials.
- Prescription from a Licensed Healthcare Provider - A detailed prescription specifying the type and necessity of the DME is required to verify medical need under federal guidelines.
- Proof of Medical Necessity - Comprehensive documentation, including patient diagnosis and treatment history, must demonstrate that the equipment is essential for the patient's health condition.
- Supplier Documentation and Compliance Records - DME suppliers must maintain signed delivery records and ensure compliance with Medicare and Medicaid enrollment and billing policies to validate the claim.
Recordkeeping and Audit Preparedness for DME Providers
Durable Medical Equipment (DME) providers must maintain accurate and comprehensive records to ensure successful reimbursement. Proper documentation supports claims and demonstrates compliance with payer requirements.
Essential documents include detailed patient records, physician prescriptions, proof of delivery, and itemized invoices. Maintaining organized files facilitates audit readiness and reduces the risk of claim denials. Your commitment to thorough recordkeeping strengthens reimbursement processes and protects against compliance issues.
What Documents are Needed for Durable Medical Equipment Reimbursement? Infographic