When filing a health insurance appeal, it is crucial to gather all relevant documents, including the denial letter from the insurer, medical records supporting the necessity of the treatment, and a detailed appeal letter explaining the grounds for the appeal. Physician notes, test results, and treatment plans further strengthen the case by providing evidence of medical necessity. Keeping copies of all correspondence with the insurance company ensures a thorough and organized appeal process.
What Documents Are Needed for Health Insurance Appeals?
| Number | Name | Description |
|---|---|---|
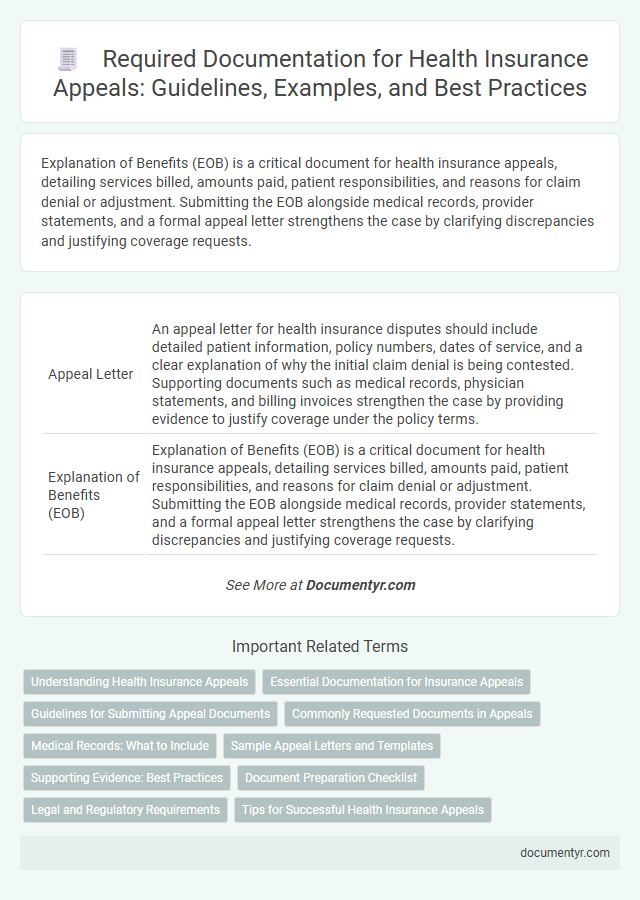
| 1 | Appeal Letter | An appeal letter for health insurance disputes should include detailed patient information, policy numbers, dates of service, and a clear explanation of why the initial claim denial is being contested. Supporting documents such as medical records, physician statements, and billing invoices strengthen the case by providing evidence to justify coverage under the policy terms. |
| 2 | Explanation of Benefits (EOB) | Explanation of Benefits (EOB) is a critical document for health insurance appeals, detailing services billed, amounts paid, patient responsibilities, and reasons for claim denial or adjustment. Submitting the EOB alongside medical records, provider statements, and a formal appeal letter strengthens the case by clarifying discrepancies and justifying coverage requests. |
| 3 | Denial Letter | The denial letter is a critical document for health insurance appeals, detailing the specific reasons for claim rejection and providing a reference number for tracking. Including this letter along with medical records, billing statements, and a written appeal increases the chances of a successful reconsideration. |
| 4 | Medical Records | Medical records are essential documents for health insurance appeals, providing detailed evidence of diagnoses, treatments, and physician notes that support the necessity of disputed medical services. These records must be comprehensive, including test results, hospital discharge summaries, and medication history to strengthen the appeal and improve the chances of a claim reversal. |
| 5 | Physician’s Letter of Medical Necessity | A Physician's Letter of Medical Necessity is a critical document for health insurance appeals, detailing the specific medical reasons and justifications for prescribed treatments or procedures. This letter must clearly explain how the requested service aligns with established medical standards and supports the patient's diagnosis to improve the chances of a successful appeal. |
| 6 | Itemized Bills | Itemized bills detailing all medical services, treatments, and procedures are essential for health insurance appeals, providing accurate evidence to support claims of coverage denial. These documents help verify charges, identify potential billing errors, and clarify the necessity of services for claim reassessment. |
| 7 | Insurance Policy Document | The Insurance Policy Document is essential for health insurance appeals as it outlines coverage details, exclusions, and claimant rights, providing a critical basis for challenging denied claims. Including this document supports a clear understanding of policy terms, ensuring the appeal aligns with the contract's provisions and strengthens the case for approval. |
| 8 | Prior Authorization Forms | Health insurance appeals require submitting prior authorization forms that verify the insurer approved the requested medical service before it was provided, ensuring compliance with policy terms. These forms serve as critical evidence in demonstrating that the necessary permissions were obtained and support the appeal for coverage reconsideration. |
| 9 | Prescription Records | Prescription records are essential documents for health insurance appeals, providing detailed evidence of prescribed medications, dosages, and treatment timelines to support the appeal case. These records validate the necessity and continuity of prescribed treatments, strengthening the claim against denial or coverage disputes. |
| 10 | Test Results | Test results play a crucial role in health insurance appeals by providing concrete medical evidence to support the claim. Accurate and detailed laboratory reports, imaging studies, and pathology findings must be submitted to substantiate the necessity of the requested treatments or services. |
| 11 | Referral Letters | Referral letters from primary care physicians or specialists serve as critical evidence in health insurance appeals by confirming the medical necessity of contested treatments or services. Including detailed referral documentation strengthens appeals by aligning the requested care with provider recommendations and insurance policy requirements. |
| 12 | Additional Supporting Documentation | Additional supporting documentation for health insurance appeals typically includes medical records, physician's letters, test results, and billing statements that clearly justify the necessity of the disputed service. Detailed clinical notes and second opinions can further strengthen the appeal by providing comprehensive evidence to counter the denial. |
| 13 | Timeline of Events | Submitting health insurance appeals requires a detailed timeline of events including the initial claim submission date, denial notification date, and subsequent correspondence dates with the insurer. Supporting documents such as medical records, denial letters, physician's notes, and proof of payment must be organized chronologically to clearly demonstrate the appeal's validity within the policy's specified time frame. |
| 14 | Communication Logs with Insurance | Comprehensive communication logs with the insurance company, including dates, times, representative names, and summaries of conversations, are essential for substantiating health insurance appeals. These records provide detailed evidence of prior correspondence and help clarify any discrepancies or misunderstandings in claim processing. |
| 15 | Copies of Previous Appeals (if any) | Copies of previous appeals are essential for health insurance appeals as they provide a documented history of prior requests and decisions, helping to establish patterns or errors in claim denials. Including detailed records such as appeal letters, response notices, and supporting evidence strengthens the case by demonstrating persistence and highlighting overlooked information. |
Understanding Health Insurance Appeals
Understanding health insurance appeals is crucial for patients seeking to challenge denied claims or coverage decisions. Proper documentation strengthens the appeal process and improves the likelihood of a favorable outcome.
- Denial Letter - This official document from the insurer outlines the reason for claim denial and serves as the basis for the appeal.
- Medical Records - Detailed clinical notes and test results provide evidence supporting the necessity of the requested treatment or service.
- Appeal Letter - A formal request written by the policyholder or healthcare provider explaining why the denial should be reconsidered.
Submitting all required documents promptly is essential to ensure timely review and resolution of health insurance appeals.
Essential Documentation for Insurance Appeals
What documents are needed for health insurance appeals? Essential documentation includes your denial letter and the original insurance policy to ensure clear understanding of the claim's rejection. Supporting medical records, bills, and physician statements strengthen your appeal by providing evidence of necessity and coverage scope.
Guidelines for Submitting Appeal Documents
Submitting an appeal for health insurance requires specific documents to support your case effectively. Essential documents include the original denial letter, detailed medical records, and a letter of medical necessity from your healthcare provider. Following the insurer's guidelines for document format and submission deadlines ensures your appeal is processed without delays.
Commonly Requested Documents in Appeals
Health insurance appeals often require specific documents to support your case effectively. Commonly requested documents include the original denial letter, medical records, and detailed billing statements.
Additional important documents are the physician's appeal letter and any prior authorization forms related to the treatment. Insurance companies may also request proof of payment and relevant correspondence between you and the insurer.
Medical Records: What to Include
Medical records play a crucial role in health insurance appeals by providing detailed evidence of your medical condition and treatments. These documents can significantly influence the outcome of the appeal when submitted accurately and thoroughly.
- Detailed Treatment Notes - Include comprehensive notes from physicians outlining diagnoses, treatment plans, and progress over time.
- Test Results and Lab Reports - Attach relevant diagnostic imaging, blood work, and laboratory analyses to support the medical necessity of treatments.
- Medication Records - Provide a list of prescribed medications, including dosages and duration, to validate prescribed therapies and care.
Sample Appeal Letters and Templates
When filing a health insurance appeal, having the right documents is crucial for a successful outcome. Key documents include the original denial letter, medical records, and a detailed appeal letter.
Sample appeal letters and templates provide structured guidance to clearly present your case. These resources help highlight important details like diagnosis, treatment necessity, and policy coverage arguments.
Supporting Evidence: Best Practices
Supporting evidence is crucial when filing health insurance appeals to prove the necessity and validity of the claim. Essential documents include medical records, doctor's notes, billing statements, and any prior authorization approvals. Organizing these records clearly and ensuring accuracy enhances the appeal's strength and improves the chances of a successful outcome.
Document Preparation Checklist
| Document | Description | Purpose |
|---|---|---|
| Appeal Letter | Formal letter outlining the reason for the appeal and reference to the denied claim | Provides a clear statement of disagreement and justification for reconsideration |
| Denial Notice | Official documentation from the insurer explaining the reason for claim denial | Serves as a reference for contested decision and grounds for appeal |
| Medical Records | Copies of relevant medical reports, test results, and physician notes | Supports the medical necessity of the treatment or service claimed |
| Explanation of Benefits (EOB) | Statement from the insurance company detailing billed charges, payments, and denials | Clarifies financial aspects and insurer's processing of the claim |
| Physician's Letter | Detailed letter from the treating physician supporting the necessity and appropriateness of care | Strengthens appeal with expert medical opinion |
| Billing Statements | Copies of invoices or bills for services or treatments | Verifies the amounts charged and services rendered |
| Additional Evidence | Supporting documents such as peer-reviewed articles or treatment guidelines | Demonstrates broader support for the treatment or service in question |
Legal and Regulatory Requirements
Health insurance appeals require specific documentation to comply with legal and regulatory standards. Proper submission of these documents ensures that appeals are processed accurately and within mandated timeframes.
- Appeal Letter - A detailed letter outlining the reason for the appeal and referencing the policy terms as required by state and federal insurance regulations.
- Medical Records - Comprehensive medical documentation supporting the claim, including physician notes and test results, which must adhere to privacy laws such as HIPAA.
- Insurance Policy Documents - Copies of the original insurance policy and any correspondence related to claim denials, necessary for verifying coverage under regulatory guidelines.
What Documents Are Needed for Health Insurance Appeals? Infographic