Patients require several key documents for chemotherapy approval, including a detailed physician's referral outlining the diagnosis and treatment plan, recent laboratory test results, and imaging reports that confirm the cancer type and stage. A comprehensive medical history and any previous treatment records help ensure accurate assessment and personalized therapy. Approval may also require insurance authorization forms and consent documentation to proceed with the chemotherapy regimen.
What Documents Does a Patient Need for Chemotherapy Approval?
| Number | Name | Description |
|---|---|---|
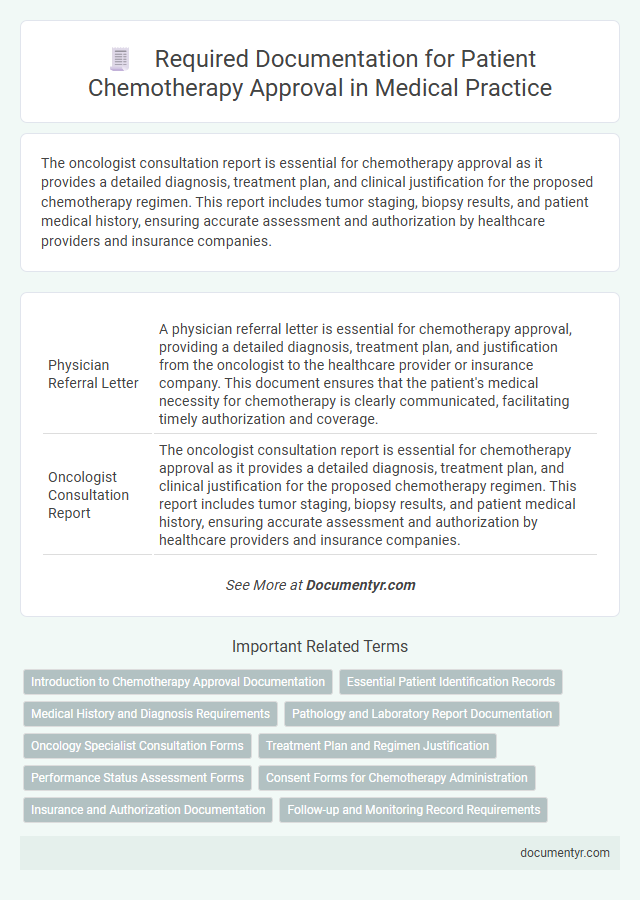
| 1 | Physician Referral Letter | A physician referral letter is essential for chemotherapy approval, providing a detailed diagnosis, treatment plan, and justification from the oncologist to the healthcare provider or insurance company. This document ensures that the patient's medical necessity for chemotherapy is clearly communicated, facilitating timely authorization and coverage. |
| 2 | Oncologist Consultation Report | The oncologist consultation report is essential for chemotherapy approval as it provides a detailed diagnosis, treatment plan, and clinical justification for the proposed chemotherapy regimen. This report includes tumor staging, biopsy results, and patient medical history, ensuring accurate assessment and authorization by healthcare providers and insurance companies. |
| 3 | Pathology Report | The pathology report detailing the diagnosis, tumor type, and staging is essential for chemotherapy approval, providing critical evidence of the patient's medical condition. This document confirms malignancy, guides treatment decisions, and ensures insurance authorization for chemotherapy protocols. |
| 4 | Histopathology Report | A histopathology report is essential for chemotherapy approval as it provides a definitive diagnosis by analyzing tissue samples to confirm the type and stage of cancer. This document ensures that the chemotherapy regimen is tailored accurately to the patient's specific cancer pathology, increasing treatment efficacy and safety. |
| 5 | Imaging Reports (CT, MRI, PET, X-ray) | Imaging reports such as CT, MRI, PET, and X-ray scans are critical documents required for chemotherapy approval, providing detailed tumor characterization and staging essential for treatment planning. These reports must include precise measurements, lesion locations, and comparison with prior imaging to demonstrate disease progression or response. |
| 6 | Biopsy Report | A biopsy report is a critical document for chemotherapy approval as it provides detailed information about the type, grade, and stage of cancer, confirming the diagnosis and guiding the treatment plan. Oncologists and insurance providers rely on the biopsy report to verify the necessity and appropriateness of chemotherapy before granting approval. |
| 7 | Cancer Staging Report | A cancer staging report, detailing tumor size, lymph node involvement, and metastasis status, is essential for chemotherapy approval as it guides treatment planning and eligibility. This report, often supplemented by pathology and imaging findings, provides oncologists with critical information to tailor chemotherapy protocols effectively. |
| 8 | Blood Test Results | Blood test results are crucial documents required for chemotherapy approval, providing essential information on a patient's blood cell counts, liver and kidney function, and overall health status. These results help oncologists determine the patient's ability to tolerate chemotherapy and tailor treatment plans accordingly. |
| 9 | Liver Function Test (LFT) | A patient requires recent Liver Function Test (LFT) results to evaluate hepatic enzyme levels and bilirubin before chemotherapy approval, ensuring liver adequacy for drug metabolism. Accurate LFT reports help oncologists assess potential hepatotoxicity risks and tailor chemotherapy protocols accordingly. |
| 10 | Kidney Function Test (KFT) | A Kidney Function Test (KFT) report is essential for chemotherapy approval, as it provides critical data on renal parameters like serum creatinine, blood urea nitrogen, and glomerular filtration rate, ensuring patient safety during treatment. Oncologists use this information to assess kidney health and adjust chemotherapy dosage accordingly to prevent nephrotoxicity. |
| 11 | ECG/EKG Report | An ECG/EKG report is essential for chemotherapy approval as it assesses the heart's electrical activity to detect any cardiac issues that may influence treatment safety. Oncologists require this report to evaluate cardiac function and to prevent potential cardiotoxicity from certain chemotherapy drugs. |
| 12 | Echocardiogram Report (if required) | An echocardiogram report, often required for chemotherapy approval, provides critical information on cardiac function to assess the patient's heart health and potential chemotherapy risks. This detailed cardiac evaluation helps oncologists determine the safety of administering cardiotoxic agents and tailor treatment plans accordingly. |
| 13 | Prescribed Chemotherapy Protocol | A prescribed chemotherapy protocol must include detailed physician orders specifying drug names, dosages, administration schedule, and treatment duration to obtain chemotherapy approval. Supporting documents often include diagnostic reports, treatment history, and insurance authorization forms to validate the necessity of the prescribed regimen. |
| 14 | Multidisciplinary Tumor Board Recommendation | A multidisciplinary tumor board recommendation is essential for chemotherapy approval, providing a comprehensive evaluation of the patient's diagnosis, treatment plan, and prognosis by specialists across oncology, pathology, radiology, and surgery. This document ensures consensus on medical necessity, supporting insurance claims and guiding personalized chemotherapy regimens. |
| 15 | Health Insurance Approval Letter | The health insurance approval letter is a critical document that confirms coverage for chemotherapy treatments and outlines the extent of financial support provided. This letter must include detailed information such as the patient's diagnosis, prescribed chemotherapy regimen, approved treatment duration, and any pre-authorization or referral numbers required by the insurer. |
| 16 | Pre-authorization Form (Insurance) | A patient must submit a completed pre-authorization form from their insurance provider to ensure chemotherapy approval, which details the prescribed treatment plan and verifies coverage eligibility. This form typically includes physician recommendations, diagnostic reports, and insurance policy information critical for processing authorization. |
| 17 | Patient Consent Form | A patient must provide a signed Patient Consent Form for chemotherapy approval, confirming their understanding of the treatment risks, benefits, and alternatives. This essential document ensures informed consent and legal authorization to proceed with the prescribed chemotherapy regimen. |
| 18 | Medical History Record | A comprehensive Medical History Record including prior diagnoses, treatments, allergies, and current medications is essential for chemotherapy approval. This documentation enables oncologists to assess patient eligibility and tailor treatment plans effectively. |
| 19 | Allergy Documentation | Allergy documentation is critical for chemotherapy approval, requiring detailed records of any hypersensitivity reactions to medications, including the specific allergens, reaction severity, and management strategies. Accurate allergy history helps oncologists tailor chemotherapy regimens and prevent adverse drug reactions, ensuring patient safety and treatment efficacy. |
| 20 | Current Medication List | A current medication list is essential for chemotherapy approval to help oncologists assess potential drug interactions and avoid adverse effects during treatment. This list should include all prescription drugs, over-the-counter medications, supplements, and herbal remedies the patient is currently taking. |
| 21 | Financial Assistance Application (if applicable) | Patients seeking chemotherapy approval often need to submit a financial assistance application, which typically includes proof of income, insurance details, and identification documents. These materials help healthcare providers evaluate eligibility for support programs that can reduce treatment costs and ensure timely access to chemotherapy. |
Introduction to Chemotherapy Approval Documentation
Chemotherapy approval requires specific documentation to ensure that you receive the appropriate treatment. These documents help medical professionals evaluate your condition and eligibility for chemotherapy.
The most common documents include your medical history, diagnostic test results, and a detailed treatment plan from your oncologist. Laboratory reports, imaging scans, and pathology reports are also essential to confirm the diagnosis and stage of cancer. Insurance authorization forms may be required to cover the cost of chemotherapy sessions.
Essential Patient Identification Records
| Document Type | Description |
|---|---|
| Government Issued ID | Official identification such as a passport, driver's license, or national ID card to verify the patient's identity. |
| Health Insurance Card | Proof of insurance coverage needed for payment authorization and to confirm eligibility for chemotherapy treatment. |
| Medical Record Number (MRN) | A unique identifier assigned by the healthcare provider, used to access your medical history and treatment plans. |
| Photograph ID | A recent photo attached to the medical file to ensure proper patient matching during treatment. |
| Contact Information | Current address, phone number, and emergency contacts required for communication and coordination during chemotherapy. |
Medical History and Diagnosis Requirements
Patients seeking chemotherapy approval must provide a comprehensive medical history, including prior treatments, allergies, and any concurrent medical conditions. Detailed records of previous cancer treatments, surgeries, and medications are essential to ensure safe and effective therapy planning.
Accurate and confirmed diagnosis documentation is critical, often requiring pathology reports, imaging studies, and biopsy results. These documents verify cancer type, stage, and molecular markers, guiding oncologists in selecting the appropriate chemotherapy regimen.
Pathology and Laboratory Report Documentation
Approval for chemotherapy requires precise documentation from pathology and laboratory reports. Your medical team relies heavily on these reports to determine treatment eligibility and plan.
- Pathology Report - Confirms diagnosis with detailed analysis of biopsy samples.
- Complete Blood Count (CBC) - Assesses overall blood health and suitability for chemotherapy.
- Biochemical Profile - Evaluates liver and kidney function, crucial for chemotherapy safety.
Oncology Specialist Consultation Forms
What documents are required from an oncology specialist for chemotherapy approval? Oncology specialist consultation forms must include detailed patient history and diagnostic results. These forms provide essential information for treatment planning and insurance authorization.
Treatment Plan and Regimen Justification
For chemotherapy approval, a comprehensive treatment plan is essential. This document outlines the cancer type, stage, and proposed chemotherapy protocol tailored to the patient's condition.
Regimen justification provides detailed reasoning for the selected chemotherapy drugs and dosing schedules. It demonstrates evidence-based support for the chosen therapy to ensure efficacy and safety.
Performance Status Assessment Forms
Performance Status Assessment Forms are critical documents required for chemotherapy approval. These forms evaluate your overall physical condition and ability to perform daily activities, helping oncologists determine treatment suitability. Accurate completion of these assessments ensures appropriate chemotherapy planning and patient safety.
Consent Forms for Chemotherapy Administration
Consent forms are essential documents required for chemotherapy approval, ensuring that patients are fully informed about the treatment. These forms confirm the patient's understanding and agreement to proceed with the chemotherapy regimen prescribed by their oncologist.
- Informed Consent Form - Details the chemotherapy plan, potential side effects, and alternative treatment options for the patient.
- Risk Acknowledgment - Confirms the patient acknowledges the risks and possible complications associated with chemotherapy.
- Authorization for Treatment - Grants legal permission for healthcare providers to administer chemotherapy as per the treatment protocol.
Healthcare facilities require signed consent forms to comply with legal and medical standards before initiating chemotherapy treatment.
Insurance and Authorization Documentation
Patients undergoing chemotherapy require specific documentation to obtain insurance approval and authorization. Proper paperwork ensures timely access to treatment and prevents coverage delays.
- Insurance Card - A valid insurance card verifies patient eligibility and coverage details for chemotherapy treatments.
- Pre-Authorization Form - This form, often required by insurance companies, confirms approval for chemotherapy based on medical necessity.
- Physician's Treatment Plan - Detailed documentation from the oncologist outlining the chemotherapy regimen supports the authorization process.
What Documents Does a Patient Need for Chemotherapy Approval? Infographic