Essential documents for hospital admission include a valid government-issued ID, health insurance card, and a referral or admission form from a healthcare provider. Medical records such as previous test results, vaccination history, and current medication lists are crucial for informed treatment. Emergency contact information and advance directives or consent forms help ensure patient safety and proper care coordination.
What Documents Are Necessary for Hospital Admission?
| Number | Name | Description |
|---|---|---|
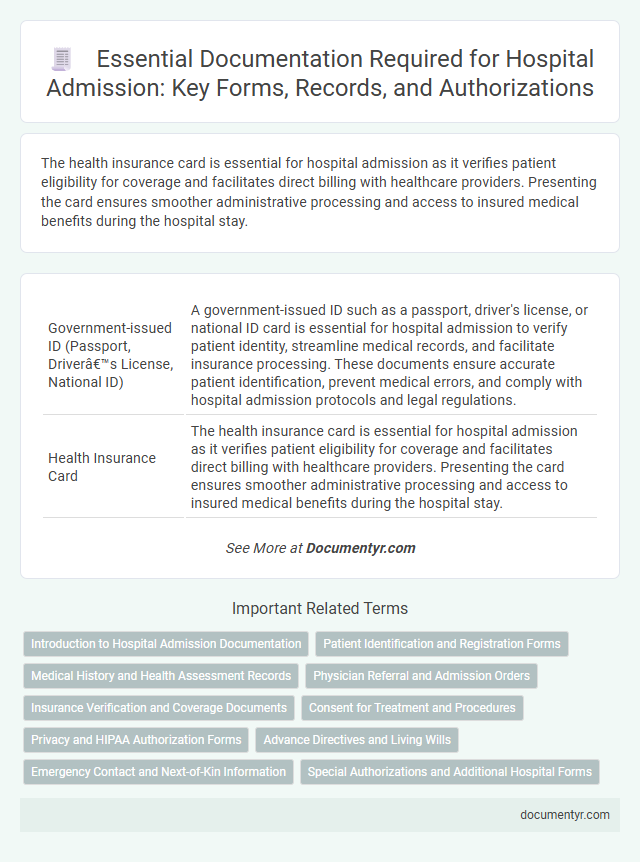
| 1 | Government-issued ID (Passport, Driver’s License, National ID) | A government-issued ID such as a passport, driver's license, or national ID card is essential for hospital admission to verify patient identity, streamline medical records, and facilitate insurance processing. These documents ensure accurate patient identification, prevent medical errors, and comply with hospital admission protocols and legal regulations. |
| 2 | Health Insurance Card | The health insurance card is essential for hospital admission as it verifies patient eligibility for coverage and facilitates direct billing with healthcare providers. Presenting the card ensures smoother administrative processing and access to insured medical benefits during the hospital stay. |
| 3 | Admission Form | The hospital admission form is a critical document containing patient identification, medical history, insurance information, and consent for treatment, ensuring accurate and efficient processing. It must be completed thoroughly to facilitate proper care coordination and comply with hospital policies and legal requirements. |
| 4 | Referral Letter (from treating physician) | A referral letter from the treating physician is essential for hospital admission as it provides a detailed medical history, diagnosis, and reason for hospitalization, ensuring appropriate care and treatment planning. This document facilitates communication between healthcare providers and helps streamline the admission process by verifying medical necessity. |
| 5 | Previous Medical Records | Previous medical records, including discharge summaries, lab results, imaging reports, and details of past treatments, are essential for hospital admission to provide accurate patient history and facilitate informed clinical decisions. These documents ensure continuity of care, reduce redundant testing, and help healthcare providers develop personalized treatment plans. |
| 6 | Test Results and Diagnostic Reports | Test results such as blood work, imaging scans (X-rays, MRIs, CT scans), and biopsy findings are essential documents required for hospital admission to provide a comprehensive assessment of the patient's condition. Diagnostic reports from referring physicians, including electrocardiograms (ECGs) and pulmonary function tests, ensure accurate diagnosis and facilitate tailored treatment planning during the hospital stay. |
| 7 | Prescription List/Medication List | A current and comprehensive prescription list or medication list is essential for hospital admission to ensure accurate medication management and avoid drug interactions. This document should include all prescribed drugs, dosages, frequencies, and over-the-counter supplements the patient is taking. |
| 8 | Emergency Contact Details | Emergency contact details, including the full name, relationship, and phone number of a reachable person, are essential documents required for hospital admission to ensure timely communication during critical situations. Accurate emergency contact information facilitates prompt notification and coordination of care in case of urgent medical events. |
| 9 | Consent Forms | Consent forms are essential documents for hospital admission, ensuring that patients are fully informed about the treatment procedures and risks before receiving medical care. These forms legally protect both the patient and the healthcare provider by documenting the patient's voluntary agreement to the proposed interventions. |
| 10 | Advance Directive/Living Will (if available) | An Advance Directive or Living Will is essential for hospital admission as it provides explicit instructions regarding medical treatments and end-of-life care preferences, ensuring patient autonomy. Hospitals require this document, if available, to guide healthcare providers in respecting the patient's wishes during critical decisions. |
| 11 | COVID-19 Vaccination Certificate (if required) | Patients must provide a valid COVID-19 vaccination certificate during hospital admission if mandated by the facility to ensure compliance with public health protocols. This certificate typically includes vaccine type, dates of administration, and is crucial for minimizing infection risks within healthcare settings. |
| 12 | Payment Guarantee/Deposit Receipt | A Payment Guarantee or Deposit Receipt is essential for hospital admission as it confirms the patient's financial responsibility and secures the hospital's commitment to provide medical services. This document typically includes the deposit amount, payer's details, and terms of payment, ensuring transparency and smooth billing processes. |
| 13 | Maternity Record (for OB/GYN admission) | A maternity record is essential for hospital admission during obstetric or gynecological care, containing critical information such as prenatal history, ultrasound results, and previous pregnancy complications. This document ensures accurate monitoring of both maternal and fetal health, facilitating timely medical interventions and personalized treatment plans. |
| 14 | Immunization Records (for pediatric patients) | Immunization records are critical for pediatric hospital admission, providing essential documentation of a child's vaccination history to ensure appropriate care and infection control. These records help healthcare providers assess immunity status and comply with public health guidelines, reducing the risk of vaccine-preventable diseases during hospitalization. |
| 15 | Guardianship/Custody Documents (for minors) | Guardianship or custody documents are essential for hospital admission of minors to establish legal authority for medical decisions and consent. These documents typically include court orders or legal guardianship papers that verify the individual's right to authorize treatment and access the minor's health records. |
| 16 | Worker’s Compensation Authorization (if applicable) | Worker's Compensation Authorization is essential for hospital admission when the injury or illness is work-related, ensuring that medical expenses and treatment are covered by the employer's insurance. Patients must provide official authorization forms or claim numbers from their employer or insurance carrier to expedite hospital processing and billing. |
| 17 | Employer Authorization/Letter (for occupational injuries) | Employer authorization letters for hospital admission in cases of occupational injuries must explicitly state the nature of the injury, confirmation of employment, and approval for medical treatment coverage. These documents ensure proper billing coordination between the hospital and the employer's workers' compensation or insurance provider. |
| 18 | Power of Attorney (if patient is incapacitated) | For hospital admission, essential documents include identification, insurance information, and medical history, with a Power of Attorney required if the patient is incapacitated to authorize medical decisions. The Power of Attorney document must be legally valid, specifying the designated individual's authority to consent to treatment and access medical records on behalf of the patient. |
| 19 | Legal/Insurance Authorization Letter (if third-party handling) | A legal or insurance authorization letter is essential for hospital admission when a third party manages the patient's payments or medical decisions, ensuring the hospital receives formal consent to proceed with treatment. This document must explicitly grant the third party the authority to handle insurance claims and authorize medical procedures on behalf of the patient. |
Introduction to Hospital Admission Documentation
| Introduction to Hospital Admission Documentation | |
|---|---|
| Purpose of Admission Documents | Hospital admission documents provide essential patient information, ensuring accurate diagnosis, treatment, and coordinated care throughout the hospital stay. |
| Key Documents Required | Identification proof, health insurance cards, referral letters, prior medical records, and consent forms are critical for validating patient identity and medical history. |
| Patient Identification | Government-issued ID such as a driver's license or passport confirms personal identity and facilitates administrative processing. |
| Health Insurance Information | Insurance policies or cards ensure coverage verification and guide billing procedures during the hospital stay. |
| Medical History Documentation | Previous medical reports, medication lists, and referral letters provide a detailed clinical background for better treatment planning. |
| Consent and Authorization Forms | Signed consent forms authorize medical procedures and protect both patient rights and hospital liability. |
| Emergency Contact Information | Contact details for family members or caregivers allow prompt communication in case of emergencies. |
| Importance of Complete Documentation | Accurate and complete admission documents reduce administrative errors, enable efficient patient evaluation, and ensure compliance with healthcare regulations. |
Patient Identification and Registration Forms
For hospital admission, accurate patient identification is crucial to ensure proper care and treatment. Your personal identification documents, such as a valid ID or health insurance card, are required to verify your identity. Completion of registration forms containing your medical history and contact information is essential for proper record-keeping and communication during your stay.
Medical History and Health Assessment Records
Hospital admission requires specific documents to ensure a comprehensive understanding of your health status. Medical history and health assessment records play a critical role in this process.
- Medical History Report - Details previous illnesses, surgeries, allergies, and chronic conditions essential for accurate diagnosis and treatment planning.
- Recent Health Assessment Records - Includes physical examination results, vital signs, and baseline lab tests to evaluate current health status.
- Medication List - Lists all prescribed and over-the-counter medications to prevent adverse drug interactions during hospital care.
Physician Referral and Admission Orders
Physician referral is a crucial document required for hospital admission, confirming the need for inpatient care. This referral must be issued by a licensed medical professional who has evaluated your condition.
Admission orders are essential instructions from the admitting physician that detail your treatment plan and care requirements. These orders serve as official authorization for your hospital stay and guide the medical team throughout your admission.
Insurance Verification and Coverage Documents
Insurance verification and coverage documents are critical for a smooth hospital admission process. These documents confirm your eligibility and financial responsibility for medical services.
- Insurance Card - Provides proof of active health insurance and contains essential policy information.
- Pre-authorization Forms - Required for specific treatments to confirm insurer approval before admission.
- Coverage Details - Outline the extent of medical services covered, including co-pays and deductibles.
Having these documents ready ensures accurate billing and prevents delays during hospital admission.
Consent for Treatment and Procedures
Consent for treatment and procedures is a crucial document required for hospital admission. This form verifies that the patient agrees to the medical interventions proposed by healthcare providers. Hospitals use it to ensure legal compliance and safeguard patient rights during care.
Privacy and HIPAA Authorization Forms
Hospital admission requires several essential documents to ensure proper patient care and legal compliance. Privacy and HIPAA authorization forms are critical to protect patient information and authorize the sharing of medical records.
These forms confirm the patient's consent for the hospital to collect, use, and disclose health information according to the Health Insurance Portability and Accountability Act (HIPAA) regulations. Without valid HIPAA authorization, healthcare providers may face restrictions in communicating important medical data with other entities involved in the patient's care.
Advance Directives and Living Wills
Advance directives and living wills play a crucial role in hospital admission by outlining a patient's medical preferences and instructions in case they become unable to communicate. These legal documents ensure that healthcare providers follow the patient's wishes regarding treatments and interventions.
Patients must present completed advance directives and living wills during the admission process to inform hospital staff of their care preferences. These documents help prevent unwanted procedures and clarify decisions about life-sustaining treatments. Hospitals often request copies to include in the patient's medical record for easy access by the care team.
Emergency Contact and Next-of-Kin Information
When preparing for hospital admission, having accurate emergency contact and next-of-kin information is essential. This data ensures medical staff can quickly communicate with your designated individuals during critical situations.
- Emergency Contact Details - Provide the full name, phone number, and relationship of a trusted person to be contacted immediately in case of an emergency.
- Next-of-Kin Information - Include legal next-of-kin names and contact information to assist with medical decisions if you are unable to communicate.
- Updated Contact Information - Verify all phone numbers and addresses to ensure timely and effective communication throughout your hospital stay.
What Documents Are Necessary for Hospital Admission? Infographic