Hospital stay pre-authorization requires submitting specific documents, including the patient's medical records, physician's referral, and detailed treatment plan. Insurance identification and prior authorization forms must also be provided to ensure coverage approval. Accurate documentation minimizes admission delays and facilitates smoother claim processing.
What Documents are Required for a Hospital Stay Pre-Authorization?
| Number | Name | Description |
|---|---|---|
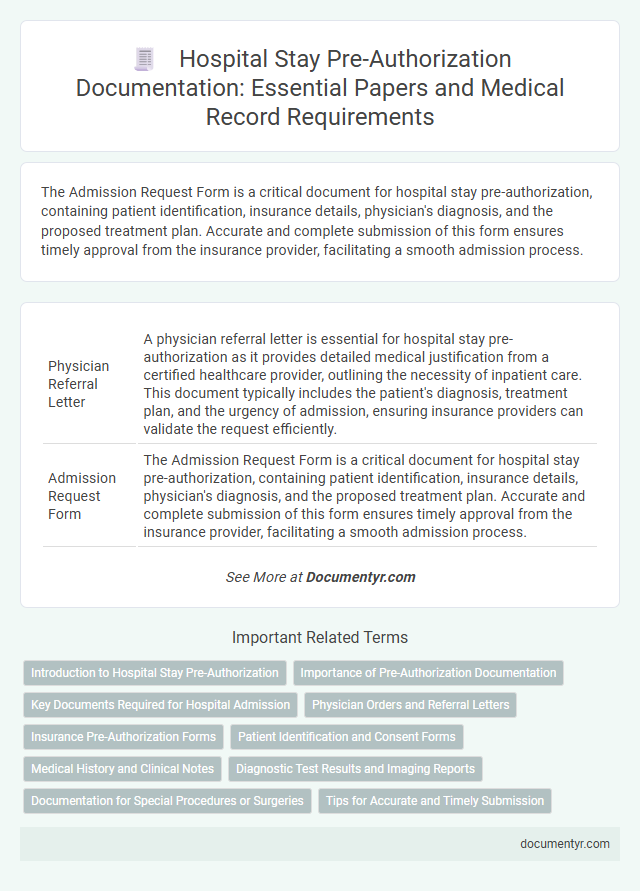
| 1 | Physician Referral Letter | A physician referral letter is essential for hospital stay pre-authorization as it provides detailed medical justification from a certified healthcare provider, outlining the necessity of inpatient care. This document typically includes the patient's diagnosis, treatment plan, and the urgency of admission, ensuring insurance providers can validate the request efficiently. |
| 2 | Admission Request Form | The Admission Request Form is a critical document for hospital stay pre-authorization, containing patient identification, insurance details, physician's diagnosis, and the proposed treatment plan. Accurate and complete submission of this form ensures timely approval from the insurance provider, facilitating a smooth admission process. |
| 3 | Patient Identification Proof | Hospital stay pre-authorization requires valid patient identification proof such as a government-issued photo ID (driver's license, passport) and insurance card to verify identity and coverage eligibility. These documents ensure accurate patient verification and facilitate the authorization process with the healthcare provider and insurer. |
| 4 | Health Insurance Policy Copy | A valid health insurance policy copy is essential for hospital stay pre-authorization as it verifies coverage details and ensures the patient's eligibility for admitted care. This document includes policy number, insured member information, and coverage limits necessary for claim processing and approval. |
| 5 | Previous Medical Records | Previous medical records, including detailed history of past treatments, diagnostic test results, and records of prior hospitalizations, are essential documents for hospital stay pre-authorization. These records enable insurance providers to verify medical necessity and authorize coverage based on comprehensive patient health information. |
| 6 | Diagnostic Test Reports | Diagnostic test reports, including blood work, imaging results, and specialist evaluations, are essential documents required for hospital stay pre-authorization to verify the necessity of inpatient care. These reports provide critical clinical evidence that supports the medical need and helps insurance providers authorize the hospital admission efficiently. |
| 7 | Clinical Summary | A clinical summary is essential for hospital stay pre-authorization, detailing the patient's medical history, diagnosis, treatment plan, and current condition. This document enables insurance providers and hospital administrators to assess the medical necessity and approve the required inpatient care promptly. |
| 8 | Proposed Treatment Plan | A detailed proposed treatment plan is essential for hospital stay pre-authorization, outlining the medical procedures, anticipated duration, and specific care requirements. This document must include the attending physician's diagnosis, recommended interventions, and expected outcomes to facilitate insurance approval and ensure comprehensive patient care coordination. |
| 9 | Pre-Authorization Request Form | The Pre-Authorization Request Form is a critical document required for hospital stay pre-authorization, containing patient information, diagnosis details, and the proposed treatment plan. This form must be accurately completed and submitted to the insurance provider to ensure approval for inpatient services and avoid claim denials. |
| 10 | Consent for Information Sharing | Consent for information sharing is a crucial document required for hospital stay pre-authorization, enabling healthcare providers to legally share patient medical records with insurance companies and specialists. This consent ensures compliance with HIPAA regulations and facilitates efficient verification of coverage and approval for hospital services. |
| 11 | Attending Physician’s Prescription | The attending physician's prescription is a critical document for hospital stay pre-authorization, detailing the medical necessity of admission and specific treatments required. This prescription must include the physician's credentials, diagnosis, proposed procedures, and anticipated duration of hospitalization to ensure insurance approval and coverage. |
| 12 | Hospital Estimate/Quotation | A hospital stay pre-authorization requires a detailed hospital estimate or quotation outlining the anticipated medical procedures, duration of stay, and associated costs. This document helps insurance providers assess coverage eligibility and approve the necessary funds before admission. |
| 13 | Employer/Corporate Authorization Letter (if applicable) | An Employer/Corporate Authorization Letter is required for hospital stay pre-authorization when the patient's medical expenses are covered or coordinated through their employer or corporate insurance plan. This letter must include the employee's details, authorization for treatment, coverage limits, and contact information for the corporate benefits administrator to facilitate claim verification and billing. |
| 14 | Valid Government ID | A valid government ID, such as a driver's license, passport, or state-issued identification card, is essential for hospital stay pre-authorization to verify patient identity and insurance eligibility. Hospitals often require this document alongside insurance cards and medical records to ensure accurate processing and approval of hospital admission. |
| 15 | Third-party Administrator (TPA) Card (if insured) | A hospital stay pre-authorization requires presenting a valid Third-party Administrator (TPA) card, which confirms insurance coverage and facilitates direct billing between the hospital and insurer. This card must include policy details and the insured's identification to ensure seamless approval and processing of medical expenses. |
| 16 | KYC Documents (if required) | Hospitals typically require KYC documents such as a government-issued photo ID (passport, driver's license), proof of address (utility bill, bank statement), and insurance card for pre-authorization of hospital stays. These documents verify patient identity and insurance eligibility, ensuring smooth processing of admission and billing. |
Introduction to Hospital Stay Pre-Authorization
Hospital stay pre-authorization is a crucial step to ensure that your medical treatment is covered by insurance before admission. It involves obtaining approval from the insurance provider based on specific documentation.
Documents required for pre-authorization typically include a physician's medical necessity statement, your insurance card, and detailed hospital admission forms. Additional paperwork might involve previous medical records, diagnostic test results, and a formal pre-authorization request submitted to your insurer. Providing accurate and complete documents helps streamline the approval process and prevents delays in your hospital stay.
Importance of Pre-Authorization Documentation
Pre-authorization for a hospital stay is essential to ensure insurance coverage and avoid unexpected expenses. Proper documentation validates the medical necessity of the procedure and expedites the approval process.
- Physician's Referral - This document confirms the need for hospitalization based on a healthcare provider's evaluation.
- Medical Reports and Test Results - Detailed clinical information supports the diagnosis and treatment plan requiring admission.
- Insurance Information - Accurate policy details enable verification of coverage and eligibility for pre-authorization.
Key Documents Required for Hospital Admission
| Key Documents Required for Hospital Admission Pre-Authorization |
|---|
| 1. Physician's Referral or Prescription A detailed referral or prescription from a licensed physician outlining the necessity for hospitalization. This document verifies the medical reason for the stay and supports the pre-authorization request. |
| 2. Health Insurance Card and Policy Details Your current health insurance card along with policy information. These details confirm your coverage and help the hospital coordinate with the insurer for authorization. |
| 3. Patient Identification Documents Government-issued ID such as a driver's license, passport, or national ID to verify your identity during the admission process. |
| 4. Medical Reports and Test Results Recent laboratory reports, diagnostic imaging, or any relevant medical documentation supporting the need for hospitalization. Includes blood tests, X-rays, MRI scans, etc. |
| 5. Pre-Authorization Form The form provided by the hospital or insurance company that requires completion and submission to initiate the pre-authorization. |
| 6. Admission Consent Forms Signed consent forms for hospital admission, treatment, and data sharing, which may be required by the hospital. |
| 7. Emergency Contact Information Contact details of a family member or legal guardian to be reached in case of emergency during your stay. |
Physician Orders and Referral Letters
Securing pre-authorization for a hospital stay requires specific medical documentation to validate the necessity of inpatient care. Physician orders and referral letters play a crucial role in this authorization process.
- Physician Orders - Detailed instructions from the attending physician outlining the required hospital services and treatment plan.
- Referral Letters - Formal recommendations from a primary care provider or specialist justifying the need for hospital admission.
- Medical Necessity Documentation - Supporting clinical notes and test results that confirm the patient's condition requires inpatient care.
Submitting accurate and complete physician orders and referral letters ensures timely approval for hospital stay pre-authorization.
Insurance Pre-Authorization Forms
Insurance pre-authorization forms are essential documents for confirming coverage before a hospital stay. These forms verify that the planned medical services meet your health insurance provider's criteria for payment.
Required information typically includes patient details, diagnosis codes, and the specific treatment or procedure planned. Submitting accurate pre-authorization forms helps avoid unexpected medical bills by ensuring insurer approval in advance.
Patient Identification and Consent Forms
What documents are required for a hospital stay pre-authorization?
Patient identification documents such as a government-issued ID or insurance card are essential to verify identity. Consent forms signed by the patient authorize the medical facility to proceed with treatments and billing processes.
Medical History and Clinical Notes
Medical history is a crucial document required for hospital stay pre-authorization. It provides detailed information about a patient's past illnesses, surgeries, and chronic conditions that influence treatment decisions.
Clinical notes from referring physicians offer essential insights into the patient's current condition and the necessity of hospitalization. These notes include diagnostic findings, treatment plans, and observations critical for approval by insurers.
Diagnostic Test Results and Imaging Reports
Diagnostic test results are essential documents needed for hospital stay pre-authorization as they provide critical information about the patient's current health condition. Imaging reports, including X-rays, MRIs, and CT scans, offer detailed visual evidence that supports the medical necessity of hospitalization. Submitting accurate and comprehensive diagnostic and imaging documentation ensures timely approval and proper patient care management.
Documentation for Special Procedures or Surgeries
Obtaining pre-authorization for a hospital stay involving special procedures or surgeries requires specific documentation to ensure approval. Proper submission of these documents supports a smooth authorization process and timely care.
- Physician's Detailed Report - Includes the diagnosis, treatment plan, and medical necessity for the procedure or surgery being requested.
- Pre-operative Evaluation - Contains pre-surgery assessments such as lab results, imaging studies, and consultation notes.
- Consent Forms and Surgical Summaries - Provide evidence of patient consent and detailed descriptions of the planned surgical interventions.
What Documents are Required for a Hospital Stay Pre-Authorization? Infographic