Patients seeking cancer treatment authorization must provide comprehensive medical records, including diagnostic reports, pathology results, imaging scans, and previous treatment history. Authorization also typically requires a physician's referral or prescription, insurance documents, and identification proof to verify patient eligibility. Ensuring all documentation is accurate and up-to-date helps streamline approval processes and avoid delays in treatment initiation.
What Documents Does a Patient Need for Cancer Treatment Authorization?
| Number | Name | Description |
|---|---|---|
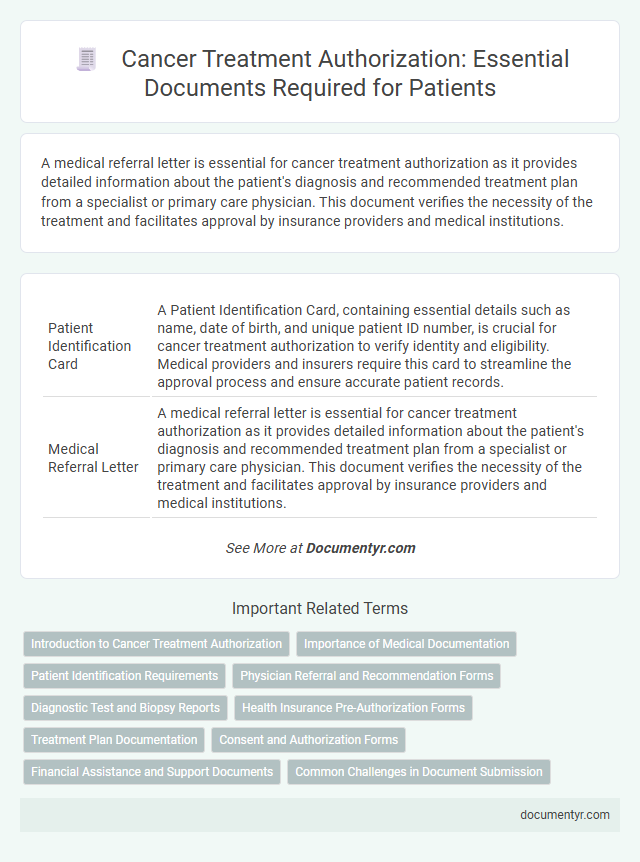
| 1 | Patient Identification Card | A Patient Identification Card, containing essential details such as name, date of birth, and unique patient ID number, is crucial for cancer treatment authorization to verify identity and eligibility. Medical providers and insurers require this card to streamline the approval process and ensure accurate patient records. |
| 2 | Medical Referral Letter | A medical referral letter is essential for cancer treatment authorization as it provides detailed information about the patient's diagnosis and recommended treatment plan from a specialist or primary care physician. This document verifies the necessity of the treatment and facilitates approval by insurance providers and medical institutions. |
| 3 | Physician’s Clinical Summary | A Physician's Clinical Summary for cancer treatment authorization must include a detailed diagnosis, clinical history, treatment plan, and relevant diagnostic test results such as pathology reports and imaging studies. This document serves as a critical component for insurance approval, demonstrating the medical necessity and urgency of the proposed cancer therapy. |
| 4 | Pathology Report | A pathology report is a critical document required for cancer treatment authorization, providing detailed information about the type, stage, and grade of the cancer based on tissue analysis. This report enables healthcare providers and insurance companies to validate the diagnosis and determine the appropriate treatment plan. |
| 5 | Imaging Reports (MRI, CT, PET, X-rays) | Patients seeking cancer treatment authorization must provide comprehensive imaging reports including MRI, CT, PET scans, and X-rays to accurately document tumor size, location, and metastasis. These diagnostic images are critical for oncologists and insurance providers to verify the diagnosis and determine the appropriate treatment plan approval. |
| 6 | Histopathology Report | A histopathology report is essential for cancer treatment authorization as it provides a definitive diagnosis by detailing the microscopic examination of biopsy tissue. This document confirms the presence, type, and grade of cancer, enabling healthcare providers and insurance companies to approve appropriate treatment plans. |
| 7 | Cancer Diagnosis Certificate | A Cancer Diagnosis Certificate detailing the specific type, stage, and date of diagnosis is essential for cancer treatment authorization as it confirms the medical necessity of proposed therapies. This certificate, issued by a licensed oncologist or cancer treatment center, serves as a primary document for insurance claims and treatment approval processes. |
| 8 | Treatment Plan (Oncologist’s Recommendation) | A patient must provide a detailed Treatment Plan from their oncologist, including specific cancer diagnosis, proposed therapies, and anticipated duration of treatment, to obtain cancer treatment authorization. This document serves as the primary evidence for insurance providers or healthcare facilities to approve and facilitate the required medical interventions. |
| 9 | Laboratory Test Results | Laboratory test results, including blood tests, biopsy reports, and imaging scans, are essential documents for cancer treatment authorization as they provide critical information about the type, stage, and progression of the cancer. Accurate and up-to-date lab results enable oncologists and insurance providers to assess the appropriate treatment plan and approve necessary medical interventions. |
| 10 | Insurance Authorization Form | A patient seeking cancer treatment authorization must provide a completed insurance authorization form, which includes detailed medical history, diagnosis codes, and the prescribed treatment plan to verify coverage eligibility. This form facilitates communication between healthcare providers and insurance companies, ensuring timely approval and minimizing delays in receiving cancer care. |
| 11 | Previous Medical Records | Previous medical records, including pathology reports, imaging studies, and prior treatment summaries, are essential for cancer treatment authorization as they provide a comprehensive overview of the patient's medical history and diagnosis details. These documents enable healthcare providers and insurance companies to verify the necessity and appropriateness of the proposed cancer therapy. |
| 12 | Consent Form for Treatment | A signed consent form for treatment is essential for cancer treatment authorization, confirming the patient's understanding of the procedure, potential risks, and alternatives. This document legally empowers healthcare providers to proceed with specific cancer therapies while ensuring patient autonomy and informed decision-making. |
| 13 | Financial Assistance Application (if applicable) | Patients applying for cancer treatment authorization may need to submit a Financial Assistance Application, which typically requires proof of income, insurance details, and identification documents. This application helps verify eligibility for financial aid programs that reduce treatment costs and ensure timely access to cancer care. |
| 14 | Prescription Orders | Prescription orders for cancer treatment authorization must include detailed information such as the patient's diagnosis, type of cancer, prescribed medications, dosage, and treatment schedule. These documents are essential for insurance approval and ensuring the patient receives timely and appropriate chemotherapy or radiation therapy. |
| 15 | Hospital Admission Form | The hospital admission form is a critical document required for cancer treatment authorization, containing patient identification, medical history, and consent details essential for hospital records. This form ensures accurate patient data collection and facilitates the approval process for specialized cancer therapies and insurance claims. |
| 16 | Government Health Scheme Card (if applicable) | Patients undergoing cancer treatment must present their Government Health Scheme Card as proof of eligibility to access subsidized or free medical services under public health programs. This card, along with identification documents and medical prescriptions, is essential for obtaining treatment authorization and ensuring coverage of diagnostic tests, chemotherapy, radiation therapy, and follow-up care. |
| 17 | Discharge Summary (if prior hospitalization) | A discharge summary is a critical document for cancer treatment authorization, detailing the patient's previous hospital stay, diagnoses, treatments administered, and clinical progress. This comprehensive report facilitates accurate assessment by oncology care providers and insurance companies, ensuring timely approval and continuity of cancer care. |
| 18 | Biopsy Report | A biopsy report is a critical document required for cancer treatment authorization, providing detailed information on the type, grade, and stage of the cancer based on tissue analysis. This report helps oncologists determine the appropriate treatment plan and is essential for insurance approval and medical record documentation. |
| 19 | Family Medical History Summary | A Family Medical History Summary is essential for cancer treatment authorization as it provides detailed information on hereditary conditions that may influence diagnosis and therapy decisions. This document typically includes records of cancer incidences, genetic disorders, and other relevant illnesses among immediate and extended family members. |
| 20 | Vaccination/Immunization Records | Patients seeking cancer treatment authorization must provide comprehensive vaccination and immunization records to demonstrate immunity status critical for treatment safety. These documents typically include history of influenza, pneumococcal, hepatitis B vaccines, and COVID-19 immunization to prevent infection risks during immunosuppressive therapies. |
Introduction to Cancer Treatment Authorization
Cancer treatment authorization is a crucial step that ensures access to appropriate medical care and insurance coverage. Understanding the required documents streamlines your approval process and reduces delays in starting treatment.
- Medical Diagnosis Report - A detailed report from your oncologist confirming the cancer type and stage.
- Insurance Coverage Application - The form submitted to your insurance provider outlining requested treatments and services.
- Physician's Treatment Plan - A comprehensive plan including proposed therapies, medications, and timelines.
Importance of Medical Documentation
What documents does a patient need for cancer treatment authorization? Comprehensive medical documentation is crucial for ensuring timely approval of cancer treatment. These documents provide a detailed history and justification for the recommended therapies.
Why is medical documentation important in cancer treatment authorization? Accurate and complete records allow healthcare providers and insurance companies to verify the diagnosis and treatment plan. This helps prevent delays and supports coverage decisions for essential cancer care.
Which specific medical documents are typically required? Commonly, you will need pathology reports, imaging results, and physician notes outlining the diagnosis and treatment recommendations. These documents establish a clear, evidence-based foundation for the authorization process.
Patient Identification Requirements
Patients seeking cancer treatment authorization must provide valid identification to verify their identity and eligibility. Commonly accepted documents include government-issued photo IDs such as a passport, driver's license, or national ID card.
Proof of residency, such as a utility bill or lease agreement, may also be required to confirm the patient's address. These identification requirements help ensure accurate patient records and facilitate insurance authorization processes.
Physician Referral and Recommendation Forms
Obtaining cancer treatment authorization requires specific documentation to ensure timely and accurate approval. Physician referral and recommendation forms are critical components in this process.
- Physician Referral Form - This document is completed by your primary care physician or oncologist to formally refer you to a cancer treatment specialist or center.
- Recommendation Letter - A detailed report from your physician explaining your diagnosis, treatment plan, and medical necessity for approval.
- Medical Records Attachment - Supporting test results, imaging studies, and pathology reports included with the referral to validate the recommended treatment approach.
Providing these accurate and comprehensive documents helps facilitate the authorization for your cancer treatment without unnecessary delays.
Diagnostic Test and Biopsy Reports
Patients seeking cancer treatment authorization must provide comprehensive diagnostic test reports. These documents include imaging studies such as CT scans, MRIs, and PET scans that confirm the presence and extent of cancer.
Biopsy reports play a critical role in the authorization process by offering a definitive cancer diagnosis through tissue analysis. Pathology results detail cancer type, grade, and molecular markers essential for personalized treatment planning. Submitting these accurate, verified reports ensures timely approval and appropriate therapeutic interventions.
Health Insurance Pre-Authorization Forms
| Document Type | Description | Purpose | Key Details |
|---|---|---|---|
| Health Insurance Pre-Authorization Form | Official form submitted to a patient's health insurance provider to obtain approval for cancer treatment services before they are rendered. | Secures insurance coverage and verifies medical necessity for specific oncology treatments, ensuring benefits apply. | Includes patient information, treatment codes (CPT/HCPCS), physician details, diagnosis codes (ICD-10), and planned procedure specifics. |
| Medical Records and Physician's Treatment Plan | Detailed documentation of the cancer diagnosis and outlined treatment protocols prepared by an oncologist. | Supports the pre-authorization request by demonstrating clinical necessity for treatments such as chemotherapy, radiation, or surgery. | Contains diagnostic test results, pathology reports, and physician's signatures. |
| Insurance Card and Patient Identification | Copies of valid insurance card and photo ID for patient verification. | Ensures accurate patient identification to prevent claim denials and facilitates communication between provider and insurer. | Includes insurance policy number, group number, and contact information. |
Treatment Plan Documentation
Patients seeking cancer treatment authorization must provide a detailed treatment plan documentation. This plan typically includes a physician's diagnosis, recommended therapies, and projected treatment timeline. Accurate and comprehensive treatment plan documentation ensures timely approval and coordinated care from healthcare providers and insurance companies.
Consent and Authorization Forms
Consent and authorization forms are essential documents required for cancer treatment approval. These forms confirm that the patient understands the treatment plan and agrees to undergo the prescribed procedures.
Patients must provide signed consent to allow medical professionals to access their health records and share information with insurance providers. Proper authorization ensures compliance with legal and institutional regulations during the cancer care process.
Financial Assistance and Support Documents
Financial assistance and support documents are crucial for securing cancer treatment authorization. These documents help verify eligibility for funding and ensure coverage for necessary medical services.
- Proof of Income - Documents such as pay stubs or tax returns demonstrate the patient's financial status for assistance qualification.
- Insurance Information - Copies of health insurance cards and policy details confirm coverage and facilitate treatment approval.
- Financial Aid Applications - Completed forms for grants or charitable assistance outline the patient's need for support during treatment.
What Documents Does a Patient Need for Cancer Treatment Authorization? Infographic