Workers' compensation medical claims require detailed documentation including the initial injury report, medical records from healthcare providers confirming the diagnosis and treatment plan, and proof of employment and work-related injury occurrence. Prescription receipts, diagnostic test results, and physician's notes outlining the extent of the injury and prognosis also play a critical role in supporting the claim. Accurate and timely submission of these documents ensures proper evaluation and processing of compensation benefits.
What Documents Are Necessary for Workers’ Compensation Medical Claims?
| Number | Name | Description |
|---|---|---|
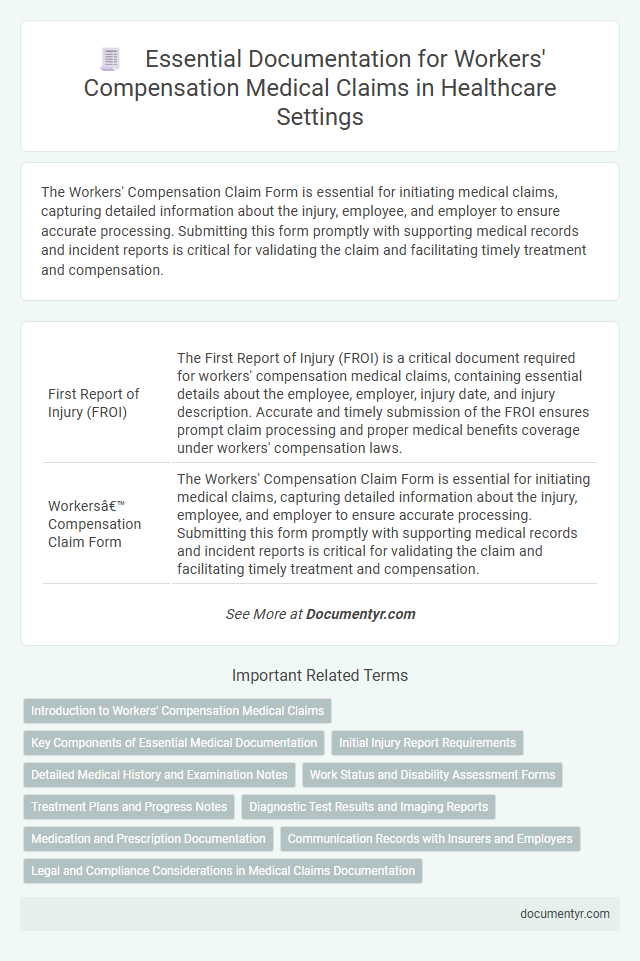
| 1 | First Report of Injury (FROI) | The First Report of Injury (FROI) is a critical document required for workers' compensation medical claims, containing essential details about the employee, employer, injury date, and injury description. Accurate and timely submission of the FROI ensures prompt claim processing and proper medical benefits coverage under workers' compensation laws. |
| 2 | Workers’ Compensation Claim Form | The Workers' Compensation Claim Form is essential for initiating medical claims, capturing detailed information about the injury, employee, and employer to ensure accurate processing. Submitting this form promptly with supporting medical records and incident reports is critical for validating the claim and facilitating timely treatment and compensation. |
| 3 | Employer’s Accident Report | The employer's accident report is a critical document for workers' compensation medical claims, detailing the incident's date, time, location, and circumstances to establish the injury's work-relatedness. Accurate and timely submission of this report ensures proper claim processing and supports the injured worker's entitlement to medical benefits and wage replacement. |
| 4 | Employee’s Statement of Injury | The Employee's Statement of Injury is a critical document detailing the circumstances and specifics of the workplace injury, essential for validating workers' compensation claims. It typically includes the date, time, location, nature of the injury, and any immediate medical treatment received, providing a foundational record for medical and legal review. |
| 5 | Medical Provider’s Initial Evaluation Report | The Medical Provider's Initial Evaluation Report is crucial for workers' compensation medical claims as it documents the patient's injury severity, medical history, and initial diagnosis, forming the foundation for treatment plans and claim approvals. This report must include detailed clinical findings, diagnostic test results, and a professional assessment to validate the work-related nature of the injury and support the claimant's entitlement to benefits. |
| 6 | Attending Physician’s Report | The Attending Physician's Report is a critical document for workers' compensation medical claims, detailing the injured employee's diagnosis, treatment plan, and prognosis. This report must include precise medical findings, dates of service, and the physician's professional assessment to ensure proper claim evaluation and timely benefits approval. |
| 7 | Work Status/Return-to-Work Form | The Work Status/Return-to-Work Form is essential for workers' compensation medical claims, documenting an injured employee's ability to resume work duties or the need for modified tasks. This form provides critical medical evaluation details from healthcare providers that guide employers and insurers in managing claim benefits and workplace accommodations. |
| 8 | Medical Bills and Invoices | Medical bills and invoices are essential documents for workers' compensation medical claims, providing detailed records of treatments, procedures, and services rendered to the injured employee. These documents must clearly itemize dates of service, provider information, treatment codes, and charges to ensure accurate processing and reimbursement. |
| 9 | Prescription Records | Prescription records are critical for workers' compensation medical claims as they provide detailed evidence of the medications prescribed and administered to the injured employee, supporting the diagnosis and treatment plan. Accurate documentation of prescription dates, dosages, and prescribing healthcare providers ensures proper evaluation of the injury's severity and the claimant's ongoing medical needs. |
| 10 | Medical Progress Notes | Medical progress notes are essential documents for workers' compensation medical claims, providing detailed records of the patient's diagnosis, treatment plan, and response to therapy. These notes ensure accurate communication between healthcare providers and claims adjusters, supporting the validity and continuity of care in the claims process. |
| 11 | Disability Certificate/Report | A Disability Certificate or Report is essential for workers' compensation medical claims as it provides official documentation of the employee's medical condition and the extent of disability resulting from the workplace injury. This document typically includes details such as diagnosis, treatment plans, and the recommended duration of work absence, serving as critical evidence to support the claim and facilitate appropriate compensation. |
| 12 | Diagnostic Test Results (e.g., X-rays, MRIs) | Diagnostic test results such as X-rays and MRIs are essential documents for workers' compensation medical claims, providing objective evidence of injuries and aiding in accurate diagnosis and treatment planning. These reports must be detailed, clearly linked to the workplace injury, and submitted promptly to support the claimant's case and facilitate timely medical benefits. |
| 13 | Functional Capacity Evaluation Report | A Functional Capacity Evaluation (FCE) report is essential for workers' compensation medical claims as it objectively assesses an injured worker's physical abilities and limitations, guiding appropriate treatment and return-to-work decisions. This detailed evaluation includes standardized testing results, job-specific functional requirements, and medical interpretations, providing critical evidence for claim approval and ongoing care management. |
| 14 | Authorization for Release of Medical Information | Authorization for Release of Medical Information is crucial in workers' compensation medical claims to allow healthcare providers to share pertinent medical records with insurers and employers; this document ensures that claims are accurately evaluated based on verified medical evidence. Without proper authorization, delays or denials may occur, hindering the claims process and affecting timely medical treatment and compensation benefits. |
| 15 | Independent Medical Examination (IME) Report | The Independent Medical Examination (IME) report is a critical document in workers' compensation medical claims, providing an impartial evaluation of the claimant's injury severity and treatment needs. This report includes detailed medical history, physical examination findings, diagnostic test results, and the examiner's professional opinion on work-related impairment and the necessity of ongoing medical care. |
| 16 | Case Management Notes | Case management notes are essential documents in workers' compensation medical claims, providing a detailed record of patient treatment, progress, and care coordination. These notes support the medical necessity of treatments, facilitate communication between healthcare providers and insurers, and help establish the legitimacy and extent of injury-related disability. |
| 17 | Rehabilitation Plan or Report | A comprehensive Rehabilitation Plan or Report is essential for workers' compensation medical claims, detailing the patient's injury, prescribed treatments, therapy sessions, progress evaluations, and estimated recovery timeline. This document ensures accurate assessment of medical necessity, supports ongoing care authorization, and facilitates proper compensation for rehabilitation services. |
| 18 | Final Medical Report/Discharge Summary | The Final Medical Report or Discharge Summary is a critical document in workers' compensation medical claims, providing a comprehensive overview of the injured worker's diagnosis, treatment, and prognosis. This report ensures accurate evaluation of the injury's extent and supports the determination of appropriate benefits and continued medical care. |
| 19 | Wage Statement or Payroll Records | Wage statements or payroll records are essential for workers' compensation medical claims as they verify the employee's earnings and establish the correct benefit amount during injury-related wage replacement. Accurate documentation of wages ensures proper calculation of indemnity payments and supports claim validity throughout the workers' compensation process. |
| 20 | Witness Statements (if applicable) | Witness statements are crucial documents in workers' compensation medical claims, providing firsthand accounts that support the claimant's injury details and work-related circumstances. These statements help validate the claim by corroborating the medical evidence and incident reports, enhancing the accuracy and credibility of the case. |
Introduction to Workers' Compensation Medical Claims
Workers' compensation medical claims require specific documentation to ensure proper processing and timely payment of medical expenses. Accurate and complete records are essential for validating injury claims and facilitating appropriate care.
- Medical Reports - Detailed physician evaluations and treatment notes documenting the injury and ongoing medical care.
- Accident Reports - Employer-provided incident descriptions confirming the circumstances and timing of the workplace injury.
- Billing Statements - Itemized invoices from healthcare providers outlining services rendered and associated costs for reimbursement.
Key Components of Essential Medical Documentation
Essential medical documentation for workers' compensation claims includes detailed injury reports and comprehensive medical evaluations. These documents establish the connection between the workplace incident and your medical condition.
Key components comprise physician's notes, diagnostic test results, and treatment plans. Accurate and thorough records ensure timely claim processing and appropriate medical care authorization.
Initial Injury Report Requirements
For workers' compensation medical claims, submitting an accurate Initial Injury Report is crucial. This document details the nature and circumstances of the injury, serving as the foundation for the claim process.
Your Initial Injury Report must include the date, time, location, and cause of the injury, along with a description of the injury itself. Medical evaluations and treatment plans from healthcare providers should accompany this report to validate the claim.
Detailed Medical History and Examination Notes
What documents are necessary for workers' compensation medical claims regarding detailed medical history and examination notes? Comprehensive medical history provides a clear record of pre-existing conditions and prior treatments relevant to the injury claim. Detailed examination notes document the current evaluation, symptoms, and clinical findings essential for accurate diagnosis and medical assessment.
Work Status and Disability Assessment Forms
Work Status and Disability Assessment Forms are critical documents in workers' compensation medical claims. These forms provide essential information on the employee's health status and ability to perform work-related duties.
- Work Status Form - Details the employee's current ability to work and any necessary restrictions or accommodations.
- Disability Assessment Form - Evaluates the extent and duration of the employee's disability related to the workplace injury.
- Medical Provider's Signature - Ensures the accuracy and authenticity of the medical evaluation documented in the forms.
Timely submission of these forms supports claim approval and appropriate management of the worker's compensation process.
Treatment Plans and Progress Notes
Treatment plans and progress notes are essential documents for workers' compensation medical claims. These records provide detailed insights into the diagnosis, prescribed therapies, and the patient's response to the treatment.
Treatment plans outline the medical procedures, medications, and rehabilitation strategies tailored to the injured worker's condition. Progress notes document ongoing evaluations, changes in symptoms, and effectiveness of interventions. You should ensure that these documents are comprehensive and regularly updated to support your claim and facilitate proper medical care.
Diagnostic Test Results and Imaging Reports
Diagnostic test results are essential documents for workers' compensation medical claims, providing objective evidence of injury or illness. Imaging reports, such as X-rays, MRIs, and CT scans, offer detailed insights into the extent of physical damage. You must include these reports to support the accuracy and validity of your medical claim.
Medication and Prescription Documentation
Medication and prescription documentation play a crucial role in workers' compensation medical claims. Accurate records ensure proper evaluation and approval of your medical treatments.
- Prescription Records - Detailed information on prescribed drugs, including dosage and frequency, validates the treatment plan.
- Pharmacy Receipts - Proof of medication purchase confirms compliance with prescribed therapies during the claim process.
- Medication Administration Logs - Documentation of medication intake supports ongoing treatment adherence and recovery assessment.
Communication Records with Insurers and Employers
Communication records with insurers and employers are essential documents for workers' compensation medical claims. These records include written correspondence, emails, and documented phone conversations that detail the claim's progress and medical treatment updates. Maintaining thorough communication ensures accurate claim processing and supports the validation of medical expenses and workplace injury reports.
What Documents Are Necessary for Workers’ Compensation Medical Claims? Infographic