To secure out-of-network medical reimbursement, patients must provide detailed medical bills, itemized receipts, and proof of payment. A physician's referral or prescription outlining the necessity of out-of-network services strengthens the claim. Patients should also submit a completed claim form from the insurance provider to ensure timely and accurate reimbursement processing.
What Documents Are Necessary for Out-of-Network Medical Reimbursement?
| Number | Name | Description |
|---|---|---|
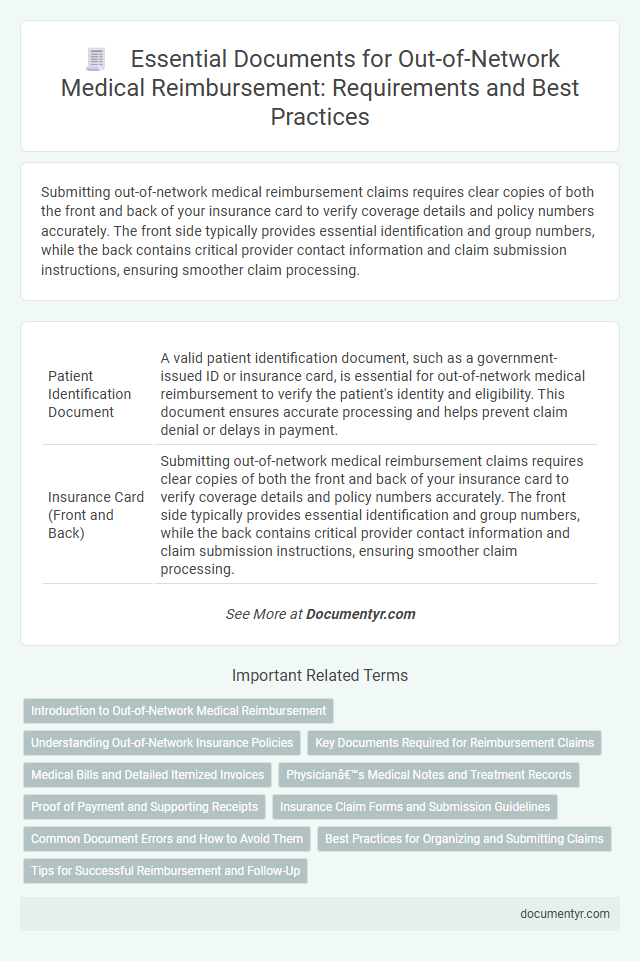
| 1 | Patient Identification Document | A valid patient identification document, such as a government-issued ID or insurance card, is essential for out-of-network medical reimbursement to verify the patient's identity and eligibility. This document ensures accurate processing and helps prevent claim denial or delays in payment. |
| 2 | Insurance Card (Front and Back) | Submitting out-of-network medical reimbursement claims requires clear copies of both the front and back of your insurance card to verify coverage details and policy numbers accurately. The front side typically provides essential identification and group numbers, while the back contains critical provider contact information and claim submission instructions, ensuring smoother claim processing. |
| 3 | Medical Bill/Invoice (Itemized) | An itemized medical bill or invoice is essential for out-of-network medical reimbursement, detailing each procedure, service date, provider information, and associated costs to ensure accurate claim processing. This document must clearly display CPT codes, diagnosis codes, quantities, and unit prices to support verification and comply with insurance requirements. |
| 4 | Payment Receipt/Proof of Payment | A payment receipt or proof of payment is essential for out-of-network medical reimbursement claims as it verifies the transaction between the patient and healthcare provider. This document must clearly show the date, amount paid, provider details, and payment method to ensure accurate processing by the insurance company. |
| 5 | Filled Reimbursement Claim Form | A filled reimbursement claim form is essential for out-of-network medical reimbursement as it provides detailed patient information, treatment specifics, and billing data required by insurance companies to process the claim accurately. Complete and accurate documentation within this form ensures timely approval and reimbursement for medical expenses incurred outside the insurance network. |
| 6 | Doctor’s Medical Report/Prescription | A detailed doctor's medical report or prescription is essential for out-of-network medical reimbursement, providing diagnosis, treatment details, and prescribed medications to validate the claim. Insurance providers require this documentation to confirm medical necessity and authorize reimbursement for services rendered outside the network. |
| 7 | Discharge Summary (if applicable) | A detailed Discharge Summary is essential for out-of-network medical reimbursement as it provides a comprehensive overview of the patient's hospital stay, diagnosis, treatment, and post-discharge instructions. Submission of this document ensures accurate verification of services rendered and supports the claim's validity. |
| 8 | Diagnosis Report | A detailed Diagnosis Report is essential for out-of-network medical reimbursement as it provides official confirmation of the medical condition requiring treatment, including ICD codes and physician's signature. This document supports the claim by validating the necessity and extent of care incurred outside the insurance network. |
| 9 | Referral Letter (if required) | A referral letter is crucial for out-of-network medical reimbursement when required by the insurance policy, as it validates the necessity of seeing a specialist outside the network. This document must be officially issued by a primary care physician or relevant healthcare provider and clearly state the medical reason for the referral to ensure claim approval. |
| 10 | Authorization Letter (if required) | An Authorization Letter is often required for out-of-network medical reimbursement to confirm prior approval from the insurance provider, ensuring the treatment or service aligns with policy terms. This document must include patient details, specific medical services requested, provider information, and explicit consent to facilitate claim processing and avoid denial. |
| 11 | Hospital/Clinic Registration Form | The Hospital/Clinic Registration Form is essential for out-of-network medical reimbursement as it verifies patient admission details, treatment dates, and hospital credentials required by insurance companies. Accurate submission of this form ensures proper claim processing and timely reimbursement for services rendered outside the insurance network. |
| 12 | Consultation Notes | Consultation notes are essential documents for out-of-network medical reimbursement, providing detailed information about the patient's diagnosis, treatment plan, and the healthcare provider's recommendations. These notes serve as proof of the medical necessity and justify the services billed, playing a crucial role in the claims review process by insurance companies. |
| 13 | Laboratory/Diagnostic Test Reports | Laboratory and diagnostic test reports are essential documents for out-of-network medical reimbursement, providing detailed evidence of medical necessity and services rendered. These reports must be accurate, include the patient's identification, test results, and the ordering physician's information to ensure successful claims processing. |
| 14 | Operative/Procedure Notes (if applicable) | Operative or procedure notes are essential documents for out-of-network medical reimbursement, providing detailed accounts of surgeries or procedures performed, including the method, duration, and any complications. These notes validate the necessity and extent of treatment, supporting insurance claims and ensuring accurate reimbursement from out-of-network providers. |
| 15 | Copy of Cheque/Bank Details (for reimbursement payment) | A copy of the cheque or detailed bank statement must be submitted to ensure accurate processing of out-of-network medical reimbursement payments. Providing clear bank details, including account number and IFSC or routing number, facilitates timely and secure transaction settlements from the insurer. |
Introduction to Out-of-Network Medical Reimbursement
Out-of-network medical reimbursement involves submitting claims for healthcare services received from providers outside your insurance network. Insurance companies typically require specific documentation to process these claims efficiently. Understanding the necessary documents ensures a smoother reimbursement experience and helps you recover eligible expenses promptly.
Understanding Out-of-Network Insurance Policies
Understanding out-of-network insurance policies is essential for securing medical reimbursement effectively. Knowing which documents are required can streamline the claim process and prevent denials.
- Itemized Medical Bills - Detailed bills from healthcare providers showing services rendered and costs are needed to verify treatment expenses.
- Proof of Payment - Receipts or bank statements demonstrating that you paid for the service confirm your financial responsibility.
- Referral or Authorization Documents - Some policies require a referral from a primary care physician or prior authorization to validate out-of-network claims.
Key Documents Required for Reimbursement Claims
Submitting a successful out-of-network medical reimbursement claim requires specific documentation to verify the services received and the expenses incurred. Key documents serve as proof of medical necessity and accurate billing information crucial for claim approval.
The primary documents include the detailed medical bills itemizing each service or procedure performed by the out-of-network provider. Additionally, patients must provide the original receipts and payment proofs confirming that the bills were settled.
Medical reports or physician's notes that validate the diagnosis and treatment are essential to demonstrate the necessity of out-of-network care. Insurance companies may also request the Explanation of Benefits (EOB) from the insurer outlining the amount covered and denied under the in-network policy.
Proper completion of claim forms with all requested personal and policy details is indispensable for prompt processing. Keeping copies of all submitted documents helps track the claim status and resolve any follow-up queries efficiently.
Medical Bills and Detailed Itemized Invoices
Medical bills are essential documents for out-of-network medical reimbursement, providing proof of the services rendered and their associated costs. These bills must clearly state the dates of service, provider information, and total charges to facilitate accurate claim processing.
Detailed itemized invoices break down each medical service and procedure, including specific codes and individual fees, helping insurers verify the legitimacy of the charges. Submitting these invoices ensures transparency and increases the likelihood of receiving appropriate reimbursement for out-of-network care.
Physician’s Medical Notes and Treatment Records
```htmlWhat documents are necessary for out-of-network medical reimbursement related to physician's medical notes and treatment records? Physician's medical notes provide detailed documentation of your diagnosis and treatment plan. Treatment records include all clinical information supporting the medical necessity of services rendered, which are crucial for reimbursement approval.
```Proof of Payment and Supporting Receipts
Submitting out-of-network medical claims requires specific documentation to ensure reimbursement. Proof of payment and supporting receipts are crucial for validating your expenses.
- Proof of Payment - Documents like credit card statements or bank statements confirming the transaction.
- Itemized Receipts - Detailed receipts showing medical services, dates, and amounts paid.
- Provider Information - Receipts must include the healthcare provider's name and contact details for verification.
Organizing these documents accurately speeds up the reimbursement process and avoids claim denials.
Insurance Claim Forms and Submission Guidelines
When filing for out-of-network medical reimbursement, insurance claim forms are essential documents that must be accurately completed. These forms capture key details about the medical services received and your insurance policy information.
Submission guidelines require attaching original itemized receipts or bills from the healthcare provider, showing procedure codes and dates of service. Detailed explanation of benefits (EOB) from your insurer may be necessary to support the claim. Carefully following these instructions ensures timely processing and reduces the risk of claim denial.
Common Document Errors and How to Avoid Them
| Document | Description | Common Errors | How to Avoid Errors |
|---|---|---|---|
| Medical Receipt or Invoice | Proof of medical services received, including dates, provider name, and charges. | Missing provider details, illegible text, or incomplete date information. | Ensure the receipt clearly states the provider's full name, service dates, and itemized costs. Request a typed or digitally issued invoice if possible. |
| Detailed Medical Report or Statement | Explanation of the diagnosis, treatment provided, and necessity of services. | Vague descriptions or absence of specific medical codes. | Request documentation that uses standardized medical codes such as ICD-10 or CPT codes. Confirm accuracy with the healthcare provider. |
| Insurance Claim Form | Official form required by your insurance company to process reimbursement. | Incomplete fields, incorrect policy numbers, or unsigned forms. | Fill out all sections carefully. Double-check policy numbers and signatures before submission. |
| Proof of Payment | Confirmation of payment made to the out-of-network provider. | Unclear payment amounts, missing dates, or ambiguous payment method. | Retain receipts with clear payment details, including date, amount, and payment method. |
| Referral or Authorization Letter (if applicable) | Document showing permission from your insurer to seek out-of-network care. | Missing authorization or expired referral. | Verify authorization status before treatment. Obtain a written referral from your insurer when required. |
Best Practices for Organizing and Submitting Claims
Submitting out-of-network medical claims requires careful preparation of specific documents to ensure timely reimbursement. Proper organization and completeness of your paperwork significantly improve the chances of claim approval.
- Itemized Medical Bills - These detailed bills should include dates of service, provider information, and a breakdown of procedures and charges.
- Proof of Payment - Receipts or bank statements verifying that you have paid the medical provider out-of-pocket are essential for reimbursement.
- Insurance Claim Form - Completed accurately with your personal and insurance information, this form is mandatory for processing your request.
What Documents Are Necessary for Out-of-Network Medical Reimbursement? Infographic