To enroll in prescription drug coverage, essential documents include a valid government-issued ID, proof of residency, and a health insurance card. Applicants must also provide income verification and any existing prescription drug plan membership details to ensure accurate processing. These documents facilitate eligibility confirmation and streamline the enrollment process for prescription drug benefits.
What Documents are Necessary for Prescription Drug Coverage Enrollment?
| Number | Name | Description |
|---|---|---|
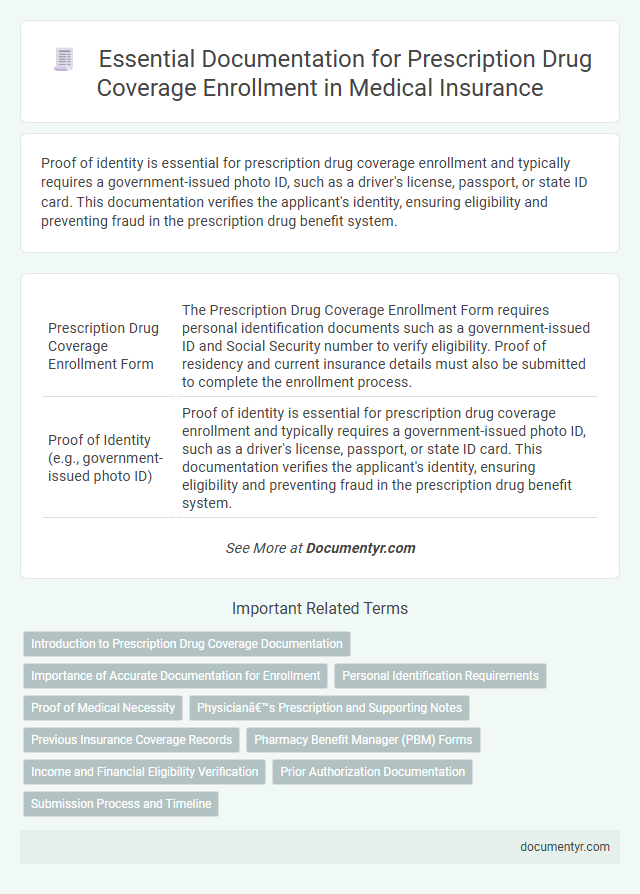
| 1 | Prescription Drug Coverage Enrollment Form | The Prescription Drug Coverage Enrollment Form requires personal identification documents such as a government-issued ID and Social Security number to verify eligibility. Proof of residency and current insurance details must also be submitted to complete the enrollment process. |
| 2 | Proof of Identity (e.g., government-issued photo ID) | Proof of identity is essential for prescription drug coverage enrollment and typically requires a government-issued photo ID, such as a driver's license, passport, or state ID card. This documentation verifies the applicant's identity, ensuring eligibility and preventing fraud in the prescription drug benefit system. |
| 3 | Proof of Address (e.g., utility bill, lease agreement) | Proof of address documents, such as a recent utility bill or a valid lease agreement, are essential for prescription drug coverage enrollment to verify the applicant's residence. These documents ensure accurate processing and eligibility confirmation within the healthcare provider's system. |
| 4 | Social Security Card or Number | Enrollment in prescription drug coverage requires providing a valid Social Security Number (SSN) to verify identity and eligibility for benefits. A Social Security Card or official documentation displaying the SSN is essential for accurate processing and preventing enrollment delays. |
| 5 | Medicare Card (if applicable) | Enrollment in prescription drug coverage requires a valid Medicare card as proof of eligibility, which displays your Medicare number and effective dates for Parts A and B. Along with the Medicare card, applicants may need to submit identification documents, proof of residency, and any current prescription drug plan information for accurate coverage activation. |
| 6 | Current Health Insurance Information | Current health insurance information, including policy numbers and coverage details, is essential for prescription drug coverage enrollment to verify eligibility and coordinate benefits. Accurate documentation helps ensure proper processing of claims and prevents delays in accessing medication benefits. |
| 7 | Proof of Income (e.g., recent pay stubs, tax returns) | Proof of income documents such as recent pay stubs, tax returns, or Social Security statements are essential for prescription drug coverage enrollment to verify eligibility and determine appropriate subsidy levels. Providing accurate income verification ensures access to cost-saving programs and prevents delays in coverage activation. |
| 8 | Proof of Citizenship or Legal Residency | Proof of citizenship or legal residency is a critical requirement for prescription drug coverage enrollment, typically verified through documents such as a valid U.S. passport, birth certificate, permanent resident card, or naturalization certificate. Insurers and government programs like Medicare and Medicaid require these documents to confirm eligibility and comply with federal regulations. |
| 9 | List of Current Medications | A detailed list of current medications, including drug names, dosages, and prescribing physician information, is essential for prescription drug coverage enrollment to ensure accurate assessment of your pharmaceutical needs. This documentation helps insurance providers tailor plan options and verify eligibility for coverage under your specific health plan. |
| 10 | Primary Care Physician Information | Primary care physician information, including the provider's name, National Provider Identifier (NPI), and contact details, is essential for prescription drug coverage enrollment to ensure proper network verification and care coordination. Providing accurate primary care physician documentation facilitates seamless prescription processing and eligibility confirmation within the insurance plan. |
| 11 | Power of Attorney or Legal Guardianship Documents (if applicable) | Power of Attorney or Legal Guardianship documents must be submitted to verify the authorized individual's capacity to enroll or make decisions on behalf of the patient for prescription drug coverage. These legal documents ensure compliance with Medicaid or Medicare enrollment requirements and protect the beneficiary's rights during prescription drug plan selections. |
| 12 | Authorized Representative Documentation (if someone is enrolling on behalf) | Authorized Representative Documentation for prescription drug coverage enrollment requires a completed, signed authorization form specifying the representative's name, relationship to the enrollee, and scope of authority. Supporting identification documents, such as government-issued IDs for both the enrollee and the authorized representative, are necessary to verify identity and prevent fraud. |
| 13 | Employer Coverage Disqualification Letter (if required) | An Employer Coverage Disqualification Letter is required when an individual's employer-sponsored health plan does not provide prescription drug coverage, serving as official proof for enrollment in alternative prescription drug plans. This document ensures eligibility verification and helps prevent coverage overlap during the prescription drug coverage enrollment process. |
Introduction to Prescription Drug Coverage Documentation
Prescription drug coverage enrollment requires specific documentation to verify eligibility and ensure accurate benefit allocation. Common documents include identification proof, insurance information, and prescription details from a healthcare provider. Understanding these requirements simplifies the enrollment process and helps you secure appropriate medication coverage efficiently.
Importance of Accurate Documentation for Enrollment
Accurate documentation is crucial for successful prescription drug coverage enrollment, ensuring that individuals receive appropriate benefits without delays. Properly submitted documents verify eligibility and prevent coverage interruptions.
- Proof of Identity - Valid identification confirms the enrollee's identity and prevents fraudulent claims.
- Insurance Information - Current insurance details are necessary to coordinate benefits and avoid overlaps in coverage.
- Medical Prescription - A valid prescription verifies the medical necessity of the drugs covered under the plan.
Ensuring all required documents are complete and precise facilitates timely processing and uninterrupted access to prescription medications.
Personal Identification Requirements
To enroll in prescription drug coverage, providing valid personal identification is essential. Documentation such as a government-issued ID establishes your identity for the enrollment process.
Acceptable forms of identification typically include a driver's license, passport, or state-issued ID card. Proof of residency may also be required to confirm eligibility. Your social security number or Medicare card is often necessary to link coverage accurately to your records.
Proof of Medical Necessity
Proof of medical necessity is a critical document required for prescription drug coverage enrollment. This document validates the need for prescribed medication based on a healthcare provider's diagnosis and treatment plan.
You must provide detailed medical records or a physician's statement confirming that the medication is essential for your health condition. Insurance providers often require this proof to approve coverage and ensure appropriate drug use.
Physician’s Prescription and Supporting Notes
Physician's prescription is essential for prescription drug coverage enrollment as it validates the medical necessity of the medication. This document must be signed by a licensed healthcare provider specifying the prescribed drugs and dosage.
Supporting notes from the physician provide detailed medical history and justification for the prescription. These notes help insurance providers verify eligibility and ensure appropriate coverage for the prescribed treatment.
Previous Insurance Coverage Records
Previous insurance coverage records are essential when enrolling in prescription drug coverage. These documents provide proof of your prior coverage and help determine eligibility and coverage gaps. Ensuring you submit accurate records can streamline the enrollment process and avoid penalties.
Pharmacy Benefit Manager (PBM) Forms
| Document Type | Description | Purpose |
|---|---|---|
| Pharmacy Benefit Manager (PBM) Enrollment Form | Official form provided by the PBM required for initiating prescription drug coverage. | Registers the beneficiary in the PBM system to manage prescription drug benefits efficiently. |
| Prescription Drug Coverage Application | Form detailing personal information, insurance details, and prescription needs. | Assists PBM in determining eligible drug coverage and benefit levels. |
| Proof of Identity | Government-issued ID such as a driver's license or passport. | Verifies the identity of the enrollee to prevent fraud in prescription drug benefits. |
| Insurance Card or Policy Document | Documentation showing current health insurance coverage. | Confirms existing coverage and integrates prescription benefits with the primary health plan. |
| Physician's Prescription or Authorization | Official prescription or prior authorization from a licensed healthcare provider. | Validates medical necessity for specific prescription drugs under PBM coverage. |
| Pharmacy Benefit Manager Agreement | Contract outlining terms between the enrollee and the PBM. | Defines rights, responsibilities, and coverage conditions for prescription drug benefits. |
Income and Financial Eligibility Verification
What documents are necessary for prescription drug coverage enrollment related to income and financial eligibility verification? You must provide proof of income such as recent pay stubs, tax returns, or bank statements. Verification ensures that your eligibility aligns with program requirements for cost assistance and coverage.
Prior Authorization Documentation
Prescription drug coverage enrollment requires specific documentation to verify medical necessity and eligibility. Prior authorization documentation is essential to ensure approval for certain medications not typically covered without special approval.
- Physician's Recommendation - A detailed letter from your healthcare provider explaining why the prescribed drug is necessary.
- Medical Records - Relevant health history and test results supporting the need for the specific medication.
- Insurance Forms - Completed prior authorization forms submitted by the healthcare provider to the insurance company.
What Documents are Necessary for Prescription Drug Coverage Enrollment? Infographic