Patients seeking medical insurance reimbursement must provide a completed authorization form from their healthcare provider, detailing the recommended treatments or procedures. Original medical reports, prescriptions, and detailed billing statements from the medical facility are essential to support the claim. Copies of valid insurance cards and identification documents are also required to verify coverage and patient identity.
What Documents Does a Patient Need for Medical Insurance Reimbursement?
| Number | Name | Description |
|---|---|---|
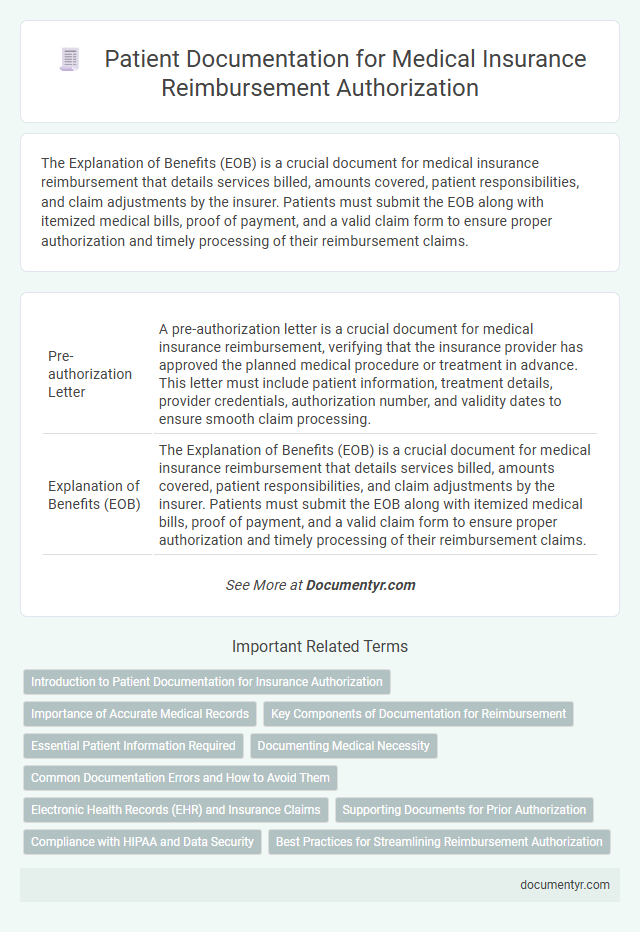
| 1 | Pre-authorization Letter | A pre-authorization letter is a crucial document for medical insurance reimbursement, verifying that the insurance provider has approved the planned medical procedure or treatment in advance. This letter must include patient information, treatment details, provider credentials, authorization number, and validity dates to ensure smooth claim processing. |
| 2 | Explanation of Benefits (EOB) | The Explanation of Benefits (EOB) is a crucial document for medical insurance reimbursement that details services billed, amounts covered, patient responsibilities, and claim adjustments by the insurer. Patients must submit the EOB along with itemized medical bills, proof of payment, and a valid claim form to ensure proper authorization and timely processing of their reimbursement claims. |
| 3 | Superbill | A patient needs to provide a Superbill, which is an itemized document issued by the healthcare provider detailing the services rendered, including CPT codes, diagnosis codes, provider information, and charges, to facilitate medical insurance reimbursement. This document is essential for insurance companies to process claims accurately and ensure reimbursement for covered medical expenses. |
| 4 | Medical Necessity Certificate | A Medical Necessity Certificate is essential for medical insurance reimbursement, as it verifies that the prescribed treatment or procedure is required for the patient's health condition according to medical standards. Insurers typically require this document, signed by a licensed healthcare provider, to validate claims and ensure coverage eligibility. |
| 5 | Cashless Authorization Form | Patients seeking medical insurance reimbursement must provide a Cashless Authorization Form, which acts as a pre-approval document allowing direct settlement of hospital bills with the insurer. This form typically requires patient identification details, policy number, and the hospital's information to facilitate seamless cashless treatment under the insurance policy. |
| 6 | Diagnostic Report Upload | Patients seeking medical insurance reimbursement must submit a detailed diagnostic report that verifies the medical necessity of the treatment or procedures performed. Accurate and complete diagnostic report uploads streamline claim processing and increase the likelihood of timely reimbursement approvals. |
| 7 | Claim Intimation Receipt | The Claim Intimation Receipt is a crucial document required for medical insurance reimbursement, serving as proof that the insurance provider has been informed about the claim. This receipt typically includes the policy number, claimant's details, and the date of claim notification, enabling a smoother and faster reimbursement process. |
| 8 | Patient Demographic Sheet | A Patient Demographic Sheet is essential for medical insurance reimbursement as it provides accurate personal information including full name, date of birth, address, contact details, and insurance policy number. This document ensures proper patient identification and streamlines the claims process by verifying eligibility and coverage details. |
| 9 | E-claim Submission Number | Patients must provide their E-claim Submission Number along with the original medical bills, prescription, and discharge summary to ensure smooth medical insurance reimbursement. This unique E-claim number is essential for tracking the claim status and verifying the authenticity of the submitted documents. |
| 10 | Digital Consent Form | Patients must provide a digital consent form that authorizes the release of medical information necessary for insurance claims, ensuring compliance with privacy laws like HIPAA. This digital document streamlines the reimbursement process by allowing healthcare providers and insurers to access and verify medical records electronically. |
Introduction to Patient Documentation for Insurance Authorization
Patients seeking medical insurance reimbursement must provide specific documentation to authorize their claims. Accurate and complete patient documentation ensures smooth processing and approval of insurance requests. Understanding the required documents helps prevent delays and facilitates timely reimbursement.
Importance of Accurate Medical Records
Accurate medical records are essential for medical insurance reimbursement, as they provide detailed documentation of the treatments and services received. These records include itemized bills, doctor's reports, and diagnostic test results, which validate the insurance claim.
You need to submit clear and precise documents to avoid delays or denials in reimbursement. Incomplete or incorrect medical records can lead to challenges in proving eligibility and medical necessity to the insurance company.
Key Components of Documentation for Reimbursement
To secure medical insurance reimbursement, key documents must include a detailed medical report, original receipts, and a valid insurance claim form. The medical report should outline the diagnosis and treatment details signed by the attending physician. Your proper compilation of these documents ensures a smooth and successful reimbursement process.
Essential Patient Information Required
To ensure smooth medical insurance reimbursement, you must submit essential patient information. This includes a valid government-issued ID, insurance policy number, and proof of treatment.
Medical reports, original bills, and prescription receipts are also necessary for verifying the claim. Accurate and complete documentation accelerates the approval and reimbursement process.
Documenting Medical Necessity
Medical insurance reimbursement requires thorough documentation of medical necessity to ensure claims are approved. Essential documents include a detailed physician's prescription, diagnostic reports, and treatment plans that justify the medical intervention.
Insurance providers typically demand comprehensive medical records, including progress notes and physician's certification, to validate the need for services or medications. Submitting original invoices, payment receipts, and claim forms facilitates smooth processing. You must ensure that all documents explicitly demonstrate the healthcare service's necessity based on your medical condition.
Common Documentation Errors and How to Avoid Them
Patients often encounter delays in medical insurance reimbursement due to missing or incorrect documentation. Understanding the necessary documents and common errors can streamline the approval process and prevent claim rejections.
Accurate and complete paperwork is essential for successful reimbursement claims in medical insurance.
- Properly Completed Claim Form - Ensure all patient and provider details are filled out correctly to avoid processing delays.
- Original Medical Bills and Receipts - Submit original or certified copies to verify the services rendered and expenses incurred.
- Doctor's Prescription and Medical Reports - Include detailed medical notes and prescriptions to justify the treatment and eligibility for reimbursement.
Electronic Health Records (EHR) and Insurance Claims
For medical insurance reimbursement, patients need specific documents to support their claims. Electronic Health Records (EHR) and insurance claims play a crucial role in this process.
- Electronic Health Records (EHR) - EHR contains comprehensive digital records of your medical history, treatments, and diagnoses required for claim validation.
- Insurance Claims Form - This form must be accurately completed with details of the medical services provided to initiate reimbursement.
- Supporting Medical Documents - Receipts, prescriptions, and referral letters are necessary to verify the expenses and treatments claimed.
Providing these documents ensures a smoother and faster medical insurance reimbursement experience.
Supporting Documents for Prior Authorization
| Document Type | Description | Purpose in Prior Authorization |
|---|---|---|
| Physician's Referral | Official referral or prescription from the attending physician specifying required medical services or treatments | Confirms medical necessity and initiates the prior authorization process |
| Medical Records | Detailed health records including diagnosis reports, lab results, imaging studies, and treatment history | Supports the clinical justification for the requested treatment or procedure |
| Insurance Claim Form | Standardized form submitted to the insurer to request coverage and payment | Facilitates processing and ensures all required patient and service details are documented |
| Prior Authorization Request Form | Form specifically designed by the insurer to request approval before service delivery | Documents the specifics of the treatment and provider for insurer review |
| Proof of Identity | Government-issued ID such as passport, driver's license, or insurance card | Verifies the patient's identity and insurance eligibility |
| Billing and Coding Information | CPT codes, ICD codes, and cost estimates related to the medical services requested | Ensures accurate service description and cost assessment during authorization |
| Supporting Physician Notes | Detailed notes from the physician explaining treatment rationale, risks, and alternatives | Strengthens the justification for prior authorization approval |
Compliance with HIPAA and Data Security
What documents does a patient need for medical insurance reimbursement while ensuring HIPAA compliance and data security? Patients typically need to provide an itemized bill, proof of payment, and a completed claim form. Your documentation must be handled with strict adherence to HIPAA regulations to protect sensitive health information and maintain data security.
What Documents Does a Patient Need for Medical Insurance Reimbursement? Infographic